
500 days of Lilly
After staying 500 days at Hamilton Health Sciences’ McMaster Children’s Hospital (MCH), one of our tiniest yet mightiest patients got to go home last November. Baby Lilly overcame many health issues with the help of her pediatric complex care team and the love and dedication of her parents.
Complications at birth
After some complications at Lilly’s birth in July 2021, first-time parents Emma Peddle and Josh Secord ended up needing more than just an overnight bag for their stay at the hospital.
Emma had been encouraged by her doctor to deliver her baby at McMaster University Medical Centre (MUMC) because of her type 1 diabetes. In case of any health issues after the birth, both mom and baby would be able to access appropriate care immediately. Lilly was born premature, at 34 weeks. Emma’s labour was prolonged and complicated because Lilly’s shoulder was stuck. This forced doctors to act fast to deliver her safely. During this process, Lilly’s left arm and clavicle (chest bone), were broken.
Lilly also had breathing issues when she was born and was admitted to the Neonatal Intensive Care Unit (NICU) at MCH, which shares a building with MUMC. She had Pyriform Aperture Stenosis, a rare birth defect where the front opening of the nose is narrow due to an overly large upper jaw bone. Two months after she was born, Lilly required intubation, which meant that a tube was inserted from her mouth into her lungs to help her breathe. During the procedure, her health-care team also recognized that one of her vocal cords was paralyzed.
Tracheostomy and training

Despite her tracheostomy, Lilly was always playful and happy.
To help Lilly with her breathing, a tracheostomy was performed when she was four months old. A tracheostomy is a hole surgeons make through the front of the neck and into the windpipe (trachea). A tracheostomy tube is placed into the hole to keep it open for breathing. This is often referred to as a “trach.” The trach can be temporary, however, it may be required longer depending on the patient’s needs.
“We were so overwhelmed and terrified,” says Emma. “We had to go through extensive training for five to six months on how to maintain and clean her trach. There’s a lot of education that goes into cleaning, putting a new one in, monitoring Lilly, and regulating her breathing.”
Part of Lilly’s tracheostomy care included suctioning. This clears the secretions from the airway so it’s easier to breathe. Lilly’s trach needed suctioning 20 to 30 times a day. The area around the tracheostomy tube was also cleaned twice a day to prevent infection and the trach tube itself needed to be changed every two weeks.
Lilly stayed in the NICU until she was six months old. Then, because of her age, size, and health concerns, she was moved to 3Z, an inpatient unit at MCH, and was on 24-hour watch in order to monitor her, and make sure she was safe.
A hospital turned home
Because of Lilly’s need to be monitored and the advanced training required to care for her, she couldn’t be released to go home until her parents learned how to care for her trach, and found at-home care during the night. The family is from Welland so it was hard to go back and forth between home and the hospital. They ended up staying at Ronald McDonald House which provided “a home away from home” for the couple.
“Other than the intense training we had to learn, we were also waiting for at-home nursing to become available for us so we could take Lilly home,” says Josh. “We needed a nurse seven days a week, for 10 hours at night or else we couldn’t bring her home.”
The duties of the home nurse included suctioning and flushing Lilly’s tubes and administering medications throughout the night, while also monitoring her heart rate and oxygen levels.
Unfortunately, COVID-19 played a factor in delaying the training sessions. Emma and Josh both caught COVID a little after Lilly’s tracheostomy surgery and could not stay at Ronald McDonald House due to their illness. This also meant they couldn’t visit Lilly.
“Like any parent, even when you’re sick you never want to leave your child,” says Emma. “As much as we were upset to leave Lilly, we had comfort in knowing the staff would provide exceptional care for her when we were gone, so we didn’t worry as much.”
It takes a village
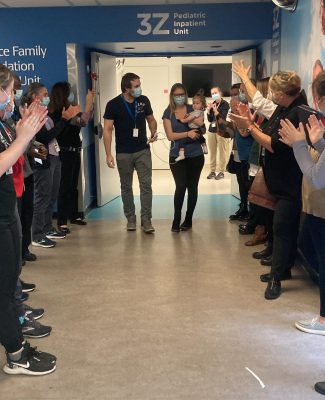
A strong turnout for the happy send-off from the staff as Lilly is released from MCH.
The pediatric complex care team is comprised of professionals from all different areas of care, including respiratory therapists (RTs), who helped with Lilly’s tracheostomy.
“Lilly’s journey was quite complex,” says Emily Oddi, one of the RTs who worked with Lilly. “She had an RT by her side from day one of her life. We worked with her whole health-care team, and seeing her progress was rewarding.”
Registered dietitians (RDs) were also part of Lilly’s team, helping her parents with her nutrition and growth. Lilly had a gastrostomy tube, or G tube, put in at the same time as her tracheostomy. Then it was changed to a Gastro-Jejunal (GJ) tube after three months to help her with her nutrition and feeding tolerance. It’s a long-term feeding option that provides more flexibility with her care and is optimal for her development and growth.
The GJ tube goes through the abdomen and ends up in two different places: the stomach for medicine and venting, and the small intestine for formula feeding. It helped to alleviate some of the symptoms of poor stomach function and reflux that had caused vomiting.
Training for the GJ tube includes learning how to dress, drain and flush it as well as how to keep the tube site clean and healthy. Lilly’s parents also had to learn how to use an infinity pump that administers formula. Usually, GJ tubes are changed every four to six months.
Occupational therapists (OTs) were also part of Lilly’s complex care team, helping to develop safe feeding skills and assist her parents in learning about the process.
“As a team, we all came together with this lens to be able to offer a baby and toddler the ability to develop – to play, feed, crawl, all those little things that are important early in life,” says OT Deborah Gjertsen. “The team as a whole had an amazing relationship with the parents. There was always excellent communication and a collaborative relationship with everyone involved.”
The sound of music

Lilly playing with musical instruments alongside her mom Emma, music therapist Bonnie Brittain, and OT Deborah Gjertsen.
One of the things Lilly enjoyed most during her time at MCH was music.
After being referred by the complex care team, MCH music therapist Bonnie Brittain worked closely with Lilly to engage her in play, play music for her, work with motor skills, and interact with musical instruments.
“Every time she would see Bonnie poke her head into the room, Lilly became so excited,” says Emma.
Brittain adds, “She was always such a social baby and remained positive through everything she went through. She went from strumming guitars to grasping maracas and shaking them. Whether singing songs or teaching new movements in play, seeing her progress and development was one of the most amazing, biggest milestones to see.”
A one-year milestone

It was a big day for Lilly and her parents when Lilly’s tracheostomy was removed.
On Nov. 9, 2022, when Lilly had been in the hospital for more than a year, her breathing, eating, and growth had stabilized enough to allow her tracheostomy to be removed and she spoke her first words. Her parents and health-care team were thrilled to learn that both her vocal cords were fully functioning.
“The family did a really beautiful job of integrating all the knowledge and skills they learned from the complex care team, and incorporating it into Lilly’s life,” says Gjertsen. “That’s a huge factor that made Lilly’s story such a successful one.”
Lilly doesn’t require her trach at all anymore and breathes completely on her own now. “She started saying mama the day after her trach had come out, her first word,” says Emma. “I was crying tears of joy, and was overwhelmed hearing her talk for the first time let alone her first word being mama.”
The hole in her throat has now completely healed and Lilly has been cleared to eat purees, take a bath in a tub, and go swimming. Emma and Josh are looking forward to having their first beach day this summer with Lilly.
A thank you that goes beyond words

Lilly in the comfort of her own home, finishing a yummy meal.
Lilly finally left the hospital on Nov. 16, 2022, 500 days after she was born. “She was always a happy baby, but we see so much more excitement in her eyes now that she is home,” says Emma.
Lilly continues to visit MCH for follow-up visits and maintenance of her GJ tube.
“We still go up to visit all the nurses on the different floors when we have follow-ups. They were such a big part of Lilly’s early life and we will never forget them,” says Josh.
Emma adds, “This is not something you plan for when you have children. Through this difficult time, we always felt reassurance and comfort from the complex care team and many staff members who helped with Lilly’s journey. It really does take a village to create a successful, happy outcome like Lilly’s, and there are not enough words to thank everyone and express our appreciation.”




