
CardiO Cycle: Not up, but moving
A change of pace
Ten years ago, hospitals around the world considered bed rest to be the best option for patients recovering from heart surgery.
“It wasn’t typical to get patients moving early in their recovery up until fairly recently,” says Anastasia Newman, a physiotherapist on ICU-West at Hamilton General Hospital (HGH). “Now, we are seeing the benefit of early movement across the health care sector, even in very ill patients.”
In healthy young adults, muscle loss can occur after only 24 hours of bed rest.
In healthy young adults, muscle loss can occur after only 24 hours of bed rest. Patients can lose between three to five per cent of muscle strength per day, and that risk increases in patients who are older or critically ill. Thanks to research, we now understand the risks of strict bed rest and the benefits of early movement, even in patients with serious complications.

Investigating early movement
Using an ergometer—a device that allows people to pedal while they’re lying in bed—is one of the simplest and safest ways to facilitate movement. As part of an overall shift to early mobility, Newman and the ICU-West team have launched a study on how this device works for patients who’ve undergone heart surgery.
“We want to study how this specific type of movement benefits our patients.”
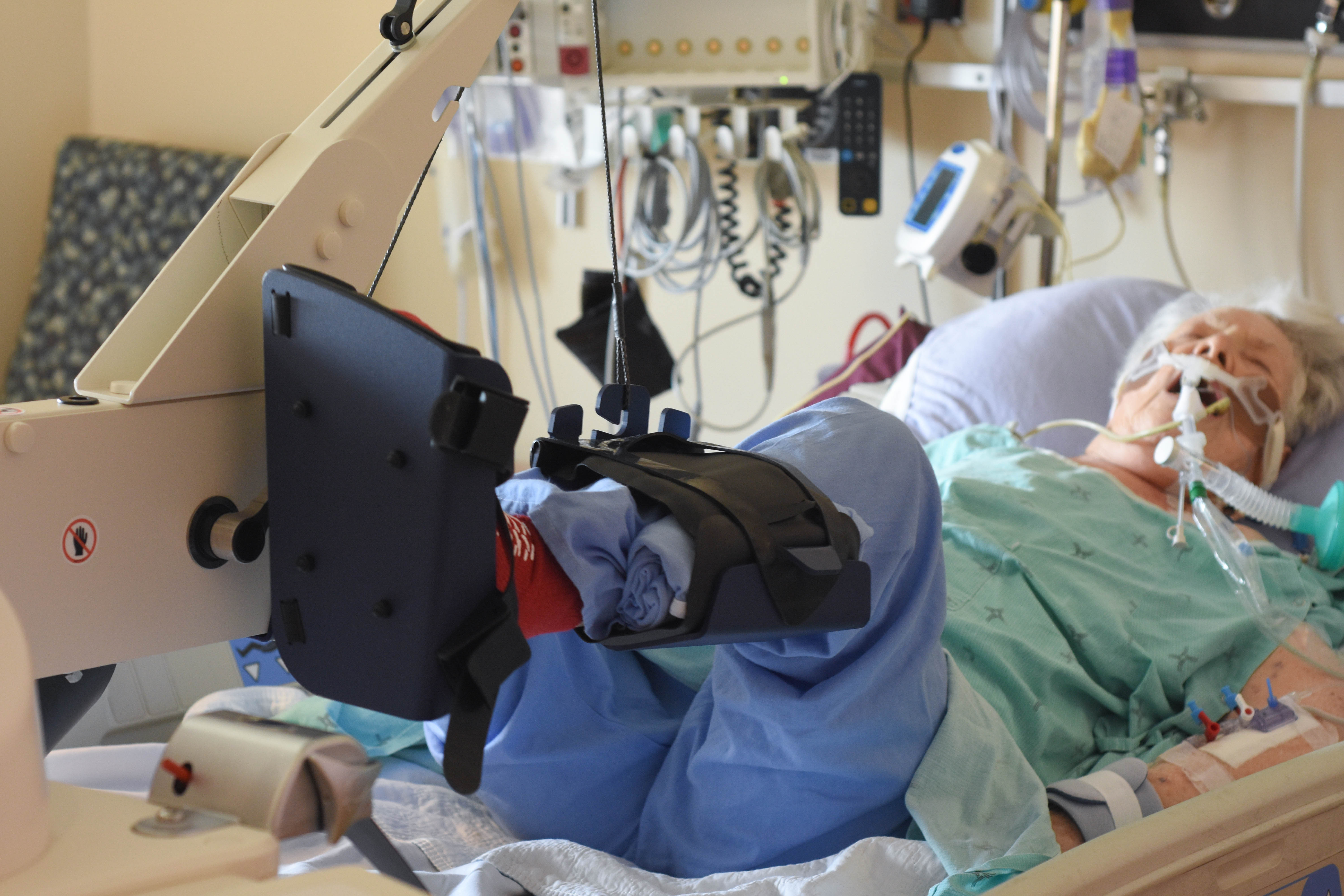
CardiO Cycle uses an in-bed cycle ergometer, brought directly to the patient’s bedside. The footboard of the bed is removed and the bike is positioned at their legs. Patients begin the therapy immediately after surgery, when they still have a tube in their airway to help them breath.
“Evaluating mobility status is part of my assessment,” says Brian Geerts, a registered nurse on ICU-West. “By working as a team, we’re able to identify when patients are ready for the ergometer and start the intervention as soon as possible.” While physiotherapists manage the sessions, nurses and respiratory therapists assist with set-up and patient monitoring.
It helps initiate lower body exercises much earlier in a patient’s stay.
One of the greatest advantages of in-bed cycling is that it allows even the sickest patients to start moving very early in their recovery. The ergometer is significantly different from other forms of exercise in that it allows for both active and passive movement. The bike can “sense” when a patient is actively exercising and will turn off its motor and allow the patient to do the work. When the patient stops actively cycling, the ergometer will start pedaling on its own, so the lower body is moving, even though the patient isn’t initiating the movement.

“If these patients can’t get out of bed, the bike allows the team to provide range of motion, strength and endurance training at the bedside,” Newman says. “It helps initiate lower body exercises much earlier in a patient’s stay.”
Expanding on findings
The ergometer has been studied in ICU patients by Dr. Michelle Kho, a clinician-scientist at St. Joseph’s Healthcare Hamilton, with positive results. Newman hopes to echo her findings in post-cardiac surgery patients, a population that hasn’t been studied in connection with this device before.

“Our hospital performs over 1800 cardiac surgeries every year—up to 40 surgeries each week. Many of our patients have the potential to fully recover, which means optimizing their quality of life post ICU stay is critically important,” says Newman.
CardiO Cycle has been designed as a pilot safety and feasibility study to see whether this type of therapy can safely be implemented in the post-cardiac ICU. If the results are positive, Newman plans to conduct a randomized controlled trial to look at long-term outcomes of using the bike.
