
Caring for COVID-19 patients: a second wave
“When we got our first COVID-19 admission, there was fear of the unknown,” says Dale Bialas, manager of the initial COVID unit at Hamilton General Hospital (HGH) during the pandemic’s first wave. As COVID-19 spread in the community, Hamilton hospitals recognized the need to consolidate COVID care and expertise in fewer, select locations. At Hamilton Health Sciences (HHS), unit “8 West” at the HGH site became the spot.
A learning experience
For some staff on the unit, this was their first job. For other, more experienced practitioners, they drew on their skills developed while working in the unit during its previous incarnation as an acute medicine unit, caring for people with serious health conditions.
In both circumstances, this new responsibility was challenging.

Dale Bialas
“The team didn’t know what personal protective equipment (PPE) was going to be available to them,” says Dale Bialas, referring to the global PPE supply shortage that resulted as hospitals, business and individuals around the world ramped up their pandemic response. “Information regarding PPE policies and guidelines were changing daily. Visitors were limited. Patients felt as if they were isolated. A lot of education had to take place.”
Nevertheless, Bialas was proud of the team’s endurance. “They were determined to show up and care for our patients.”

The team on Hamilton General Hospital’s 8 West provided care to COVID-19 patients in the Spring.
A second team
As 8 West began transitioning back to a medicine unit, the organization recognized the need for other teams to become skilled in providing care to COVID patients.

Ellen Begin
“The team on 8 West realized they were ready for others to share the responsibility,” says Ellen Begin, manager of unit 5 West at HGH, which has since become the designated COVID unit. “Our team gladly stepped up.”
With learnings from the first wave in mind, 5 West transitioned to become the COVID unit in July. In fact, they volunteered.
For now, they are part COVID unit, part medicine unit. They have created dedicated teams to care for COVID patients, and teams to care for non-COVID patients. The layout of the unit reflects this, with multiple nursing stations and washrooms to accommodate. Traffic between the two areas is limited and extra precautions are in place to protect patients and staff throughout.
The unit is newly staffed – part of a strategy to share the knowledge and equip more health professionals to care for COVID-19 patients.
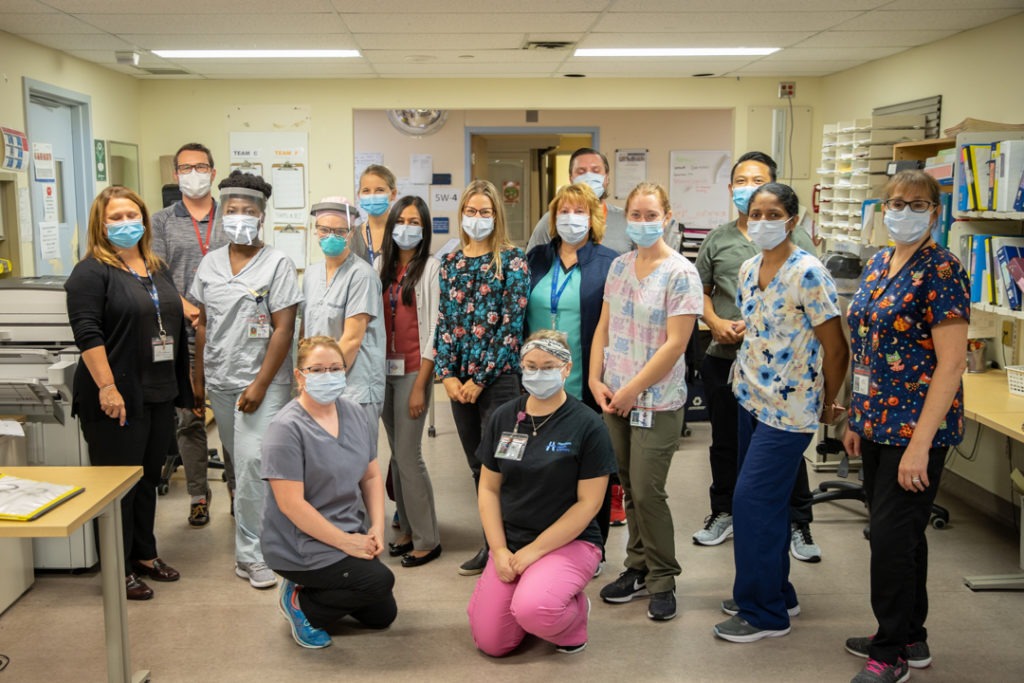
The team on Hamilton General Hospital’s 5 West volunteered to take over care of COVID-19 patients.
A toolbox
Learnings from the early stages of the pandemic has informed how the hospital continues to care for COVID-19 patients. This includes:
- Increased staff members: HHS’ Nursing Resource Team, which floats between hospital sites to provide staffing support as needed, provided staff to help on the unit. The unit was staffed above quota: a typical ratio is one nurse to 4-5 patients. During the pandemic, it was 1 nurse to 2-3 patients, depending on patients’ health conditions.
- Training for staff members: The teams received additional training in safe and appropriate use of PPE, how to care for a COVID-19 patient, proper hand hygiene practices, and much more. Clinical educators came to the unit every shift to review procedures. There was a safe space to ask questions.
- A shared model of care: In order to reduce the number of times a person has to enter a patient’s room, to decrease the number of people exposed to the virus, and to preserve PPE, the unit implemented a “shared model of care.” This means staff and physicians had to broaden their thinking to ask: “What else can we do while we’re in the room?” For instance, a doctor may pick up some of the nurse’s duties while in the patient’s room to eliminate the need for the nurse – a second body – to enter.
- Standard work to prepare rooms: The team created a checklist of standard equipment needed in a room to ensure it was stocked with the appropriate PPE, blood draw equipment, etc. This checklist acts as a visual reminder and reduces the number of times a person must enter the room.
- Ensuring safe break and lunch spaces: The team measured the lunch room on the unit to map out seats and ensure a two-meter distance between staff.
- Allowing patients to stay connected: With fewer staff entering patients’ rooms and limitations on hospital visitors, it was important to ensure patients stayed connected to their loved ones. A group of doctors delivered iPhones and tablets so that staff could help patients connect with their families virtually.
- Creating space for memorials: Jenna Pyke, a nurse on 8 West, in partnership with the Resilience team at HHS, created a memorial board to honor patients who passed away on the unit.
- Virtual appointments when possible: Advancements in virtual care now enable many patients to attend clinic appointments from the comfort of their home, helping to reduce the spread of COVID-19 in hospital.

Staff reflect on the Memorial Board to honor those who have passed
Moving forward
While Begin worked through SARS in 2013, for many HHS staff and doctors, this is their first encounter working in a pandemic.
Begin says people across HHS have embraced their essential role, like registered nurse Heather Hough.
“Becoming the COVID-19 unit has certainly been a learning experience,” says Hough. “The whole team has done a great job adapting to this new challenge together. It has been very rewarding to be able to contribute to the fight against this pandemic in such a meaningful way.”
While transmission of the virus has its ups and downs, it’s always at the forefront for those working on the unit.
“When the COVID numbers began to decrease, people didn’t talk about it that much, but our team is still living and breathing it every day,” says Begin. “For the staff on 5 West, it’s part of everyday life.
It’s scary, but I’m proud of them.”
Nurse Jenna Pyke pens letters for patients and families
 “It started with a long pause after we lost our first patient on 8 West, that I knew these would be difficult goodbyes. Patients were spending their days and nights alone all over the hospital because of new visitor rules and guidelines. Everyone understood the reasons why these rules were put in place, but it didn’t make it any easier. It didn’t make the passings any easier. As a healthcare worker, losing patients is often an expected part of the job; it’s the circle of life. We understand this basic fact, however, we work diligently every day to prevent the unfortunate outcomes. During COVID-19, losing patients hurts a little more and has stuck with us a little longer and brought us closer as a team.
“It started with a long pause after we lost our first patient on 8 West, that I knew these would be difficult goodbyes. Patients were spending their days and nights alone all over the hospital because of new visitor rules and guidelines. Everyone understood the reasons why these rules were put in place, but it didn’t make it any easier. It didn’t make the passings any easier. As a healthcare worker, losing patients is often an expected part of the job; it’s the circle of life. We understand this basic fact, however, we work diligently every day to prevent the unfortunate outcomes. During COVID-19, losing patients hurts a little more and has stuck with us a little longer and brought us closer as a team.
On 8 West, we wanted to honour and remember those who lost their lives due to this unfortunate, unfair virus. We wanted to acknowledge the lives we lost in a way that brought meaning and remembrance. When we lost a patient, we placed a lily on a memorial board in remembrance and we gathered as a team to read together a ritual of remembrance, a goodbye response reading followed by a moment of silence. The memorials have provided staff members with an opportunity to say goodbye and honour the lives of those we came to know and fought for.
This ceremony has allowed myself and the frontline staff the opportunity to grieve and obtain closure during a time when we were required to remain resilient. I wanted to show the loved ones of the patients who lost their lives to COVID-19 at HHS that we celebrated the lives they lived, we honoured them and gave them the most dignified and comfortable end of life that they deserved.”
