
Emergency doctors stepped up beyond the hospital during pandemic
“Emergency doctors at HHS have a ‘can-do’ attitude — for whatever is needed,” says Hamilton Health Sciences’ (HHS) Chief of Emergency Medicine, Dr. Kuldeep Sidhu.
More than 50 emergency department (ED) doctors work at HHS. Many have been the first point of contact for people seeking hospital care for COVID-19 symptoms.
“ED docs stepped up, even with competing priorities throughout COVID.”
While our urgent care centre was closed temporarily during the third wave (now reopened) so that staff could be redeployed to other areas where they were needed most, many physicians continued working full time in the emergency departments in addition to working in other areas such as vaccine clinics, long-term care homes and community task forces. Long hours, double shifts and fatigue were common.
“ED docs stepped up, even with competing priorities throughout COVID. The work is really remarkable. I’m amazed and grateful for their efforts,” says Sidhu.
“It isn’t just that I’m proud of them, I’m grateful that they stepped up. A lot of the times doctors weren’t even sure what they were getting into, but they volunteered for it.”
Meet three ED doctors who are making a difference beyond the walls of HHS.
Dr. Simerpreet Sandhanwalia – ensuring virtual connections and advocacy
Dr. Simerpreet Sandhanwalia co-founded two separate organizations: Frontline Connect Canada and the South Asian COVID Task Force.
“It was gut-wrenching to see our patients isolated from their loved ones.”
“Being a patient in the emergency department is often overwhelming and distressing under normal circumstances,” says Sandhanwalia. “With the advent of ‘no-visitor’ protocols brought about early in the pandemic, it was gut-wrenching to see our patients isolated from their loved ones.”
From there, Frontline Connect Canada was born. It has helped connect patients with their families virtually when stringent COVID precautions prevented visitors from entering the hospital. Technology such as iPads were obtained through community and private sector donations and distributed to those in hospital to connect with their loved ones. A related initiative, Phone Connect Canada, provided phones and SIM cards to individuals who could not afford them so they could connect with hospital or healthcare resources during the pandemic if they needed it.
Sandhanwalia also co-founded the South Asian COVID Task Force to provide COVID-19 information in different languages and advocate for increased testing centres, isolation centres and vaccine sites in hard-hit communities.
She also co-founded the national vaccine confidence campaign, This is our shot, to encourage Canadians to get vaccinated so that we can all be #TogetherAgain.
Dr. Catherine Sellens – staffing mobile vaccination clinics
Dr. Catherine Sellens participated in running mass vaccination clinics, the LTC-CARES program (more on that below), and other initiatives. But she says the most joyful experience in her 22-year career in Hamilton was vaccinating older adults at the mobile clinics in long-term care and retirement homes.
“It was an amazing opportunity to go into the community.”
Started in January 2021, the mobile clinics were tasked with going to different residences in the greater Hamilton area and vaccinating all of the clients and staff.
“It was an amazing opportunity to go into the community and to see some of these facilities, home to patients whom I had treated in the emergency department. When the group of vaccinators would arrive at one of these senior residences, there was palpable excitement by all: the vaccinators, the residents, and the staff at the facility,” says Sellens.
“As vaccinators, we were treated as heroes coming to end months of isolation and worry. The residents were so happy to see us and were patient and helpful. Many expressed their excitement at anticipated visits with their families, whom they missed so much – and I was the one they saw as ‘gifting’ this privilege to them. How lucky was I!”
“This assignment has been the most rewarding of my career and will be a memory I am grateful to hold forever.”
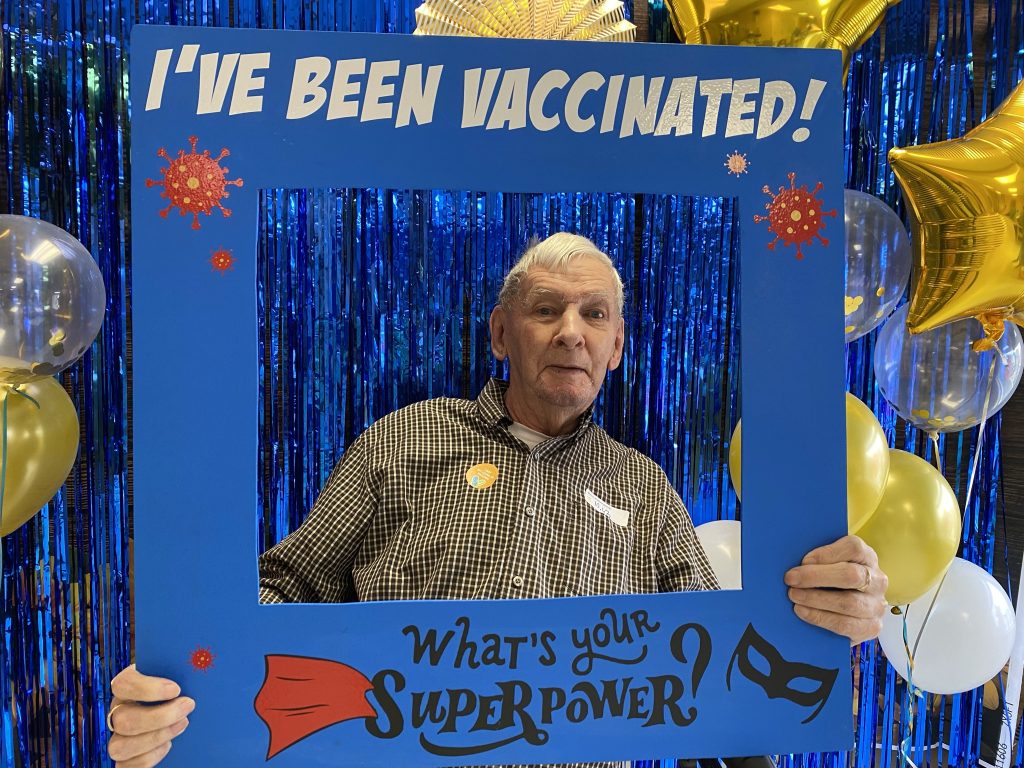
At Victoria Gardens long-term care home in Hamilton, residents like Ed could choose from a selection of selfie frames during the COVID-19 vaccination clinic and residence staff would take a photo to send to their family. “The experience was so joyful,” says Dr. Catherine Sellens.
Dr. Michelle Welsford – bringing the emergency room to long-term care homes
Dr. Michelle Welsford and an interdisciplinary team launched the LTC-CARES program in April 2020, just a few weeks into the pandemic.
“The team has been able to reduce transfers to the hospital by over 60%”
An acronym for “Consults And Recommendations for Emergency and Support Services,” the program provides care for residents inside their long-term care home, instead of having to transfer them to an emergency department.
“We recognize that providing optimal healthcare to frail elderly residents in long term care (LTC) is challenging,” says Welsford. “If quality acute care can be delivered and supported within the LTC, then care in the resident’s usual surroundings by their usual caregivers is preferred. Oftentimes this allows the resident to stay in their LTC home and receive hospital-level care without transport to hospital. ”
The program manages injuries from falls, medical device problems (such as feeding tubes) and acute health issues such as pneumonia by providing imaging, laboratory, and consultation services outside of the hospital in a mobile format.
As a result, the team has been able to reduce transfers to the hospital by over 60% and reduce admissions. They are planning to continue and have expanded the program to include other complex continuing care centres and retirement homes.
What were our ED docs up to?
Here are some of the initiatives our doctors were involved with in the community during the pandemic, outside of their usual roles in the ED:
- Working in the COVID ICUs at Juravinski Hospital and Hamilton General Hospital, and in Brantford, to support the patients and staff in those areas
- Assisting in the HHS Vaccination Centre throughout the vaccine roll-out, as well as mobile and pop-up clinics in Hamilton
- Setting up the Regional Critical Care Transport Team on the ground to transport COVID patients between hospitals when the Ornge air ambulance was busy
- Setting up the Virtual Urgent Care Centre and LTC-CARES projects to care for patients who require urgent care virtually
- Creating the Code Blue Response Teams at Juravinski Hospital and Hamilton General Hospital to respond to medical emergencies
- Working in community emergency departments funded through Health Force Ontario
- Setting up the Embassy Grand COVID Testing Center in Brampton, a center that did not require a health card for testing residents
- Setting up the National South Asian Task Force that targeted high prevalence COVID communities







