Managing COPD flare-ups
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a lung disease that develops slowly over time. It is usually diagnosed after 40 years of age, and is a long-term condition. COPD cannot be cured, but it can be treated. With proper treatment, people with COPD can lead active lives and live for many years.
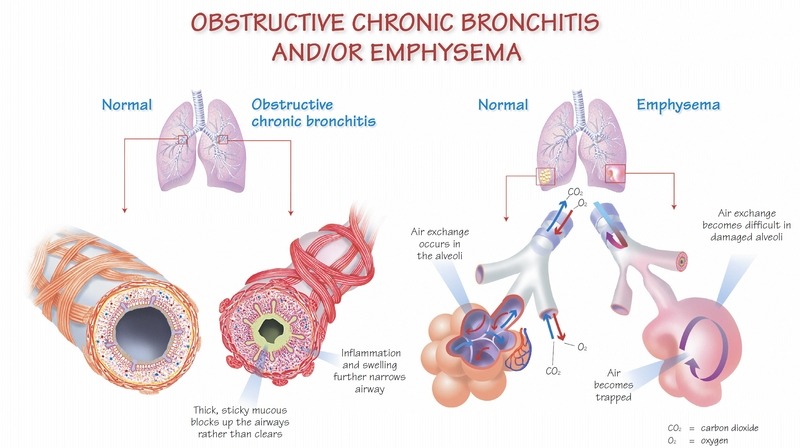
COPD includes chronic bronchitis and emphysema. Some people have one or the other, but some may have both. COPD makes it hard to move new air (oxygen) into your lungs and stale air (carbon dioxide) out.
In chronic bronchitis, difficulty breathing is caused by swelling and mucus in your airways, which blocks air from passing through. This makes you cough, expel mucous, and feel short of breath.
In emphysema, difficulty breathing is caused by damage to the air sacs at the tips of your breathing tubes. These sacs are stretchy – they stretch out when you breathe in, and shrink as you breathe out. Emphysema makes them stiffer. They don’t stretch and shrink as they should, so stale air gets trapped in your lungs. This makes you work much harder to take in air, making you feel tired and short of breath.
In most cases, COPD is a result of smoking (80-90% of cases). Other causes include genetics, exposure to dust or chemicals, second-hand smoke, frequent lung infections as a child, and exposure to wood smoke.
Managing your COPD
Getting a diagnosis early, making positive lifestyle changes, and taking appropriate medications can help you lead a normal, active life with COPD. Attending your medical appointments is very important. Ask you doctor if a Pulmonary Rehabilitation program is right for you.
If you smoke, quitting is the most important step in treating your COPD. If you need help quitting, call Smoker’s Helpline at 1-877-513-5333 or visit www.smokershelpline.ca.
Consider joining a local support group to learn more about managing your COPD. Email info@lungontario.ca for locations near you.
COPD flare-ups
A flare-up, also known as an exacerbation or “lung attack,” happens when your normal day-to-day symptoms get worse over a short period of time (a few hours to 48 hours), or when new symptoms appear. Flare-ups can be caused by a trigger, such as air pollution, scents, or allergens, or by a lung infection caused by a virus or bacteria.
Flare-ups can cause further damage to your lungs. They’re one of the main reasons people with COPD have to be hospitalized, and can be deadly.
You need to pay attention to your normal day-to-day symptoms in order to recognize a change that could indicate a flare-up. For instance: how breathless are you on a good day, how much do you cough, if you have mucus, what is the amount, thickness, stickiness of it?
Managing COPD flare-ups
There are four main steps to managing flare-ups: preventing, recognizing, beginning treatment, and seeking professional help.
1. Preventing Flare- Ups
To reduce your risk of COPD flare ups:
• Eat healthy foods.
• Exercise regularly.
• Get enough sleep.
• Find ways to make daily tasks easier.
• Avoid exposure to triggers such as air pollution, scents, and allergens whenever possible.
• Wash your hands properly before touching your eyes, nose, or mouth to avoid picking up and spreading germs.
• Stay away from people who are sick.
• Take all of the medications prescribed by your doctor.
• Practice any breathing exercises recommended by your healthcare team.
• Ask for help if you have questions about how or when to take medications or what they’re for.
• Ask your doctor for a personalized written COPD action plan.
• Get your flu shot every year.
• Ask your doctor if you need a pneumonia shot.
• Quit smoking and avoid second-hand smoke.
2. Recognizing Flare-Ups
The top three signs of a flare-up are:
• Increased cough
• Unusual increase in shortness of breath (even if just with activity)
• Increase in the amount, thickness, or stickiness of your mucus, which may be more yellow, green, or brown than usual
Other common signs include:
• Fever
• Symptoms of a cold, such as headache, sore throat, or runny nose
• Swollen ankles or unusual weight gain
• Feeling generally unwell and tired
3. How to Begin Treatment
Never wait more than one day to take action. Follow the advice written in the COPD action plan which was developed specifically for you. If you do not have written action plan similar to the example at the link above, be sure to ask your doctor for one.
4. When to call your doctor
Follow the directions in your COPD action plan, and never wait more than two days to call your doctor if you suspect a flare-up.
If you are experiencing any of these signs, call 9-1-1 immediately:
• Chest pain
• Blue lips or fingers
• Confusion, you can’t think clearly, or are very agitated or upset
• Drowsiness or sleeping a lot
• Extremely short of breath
For more information on COPD, contact the Lung Health Info Line to be connected to a certified respiratory educator. From Monday through Friday, 8:30am – 4:30pm call 1-888-344- LUNG (5864), or email info@lungontario.ca any time.
You can also visit the Lung Association OR Living Well with COPD.