
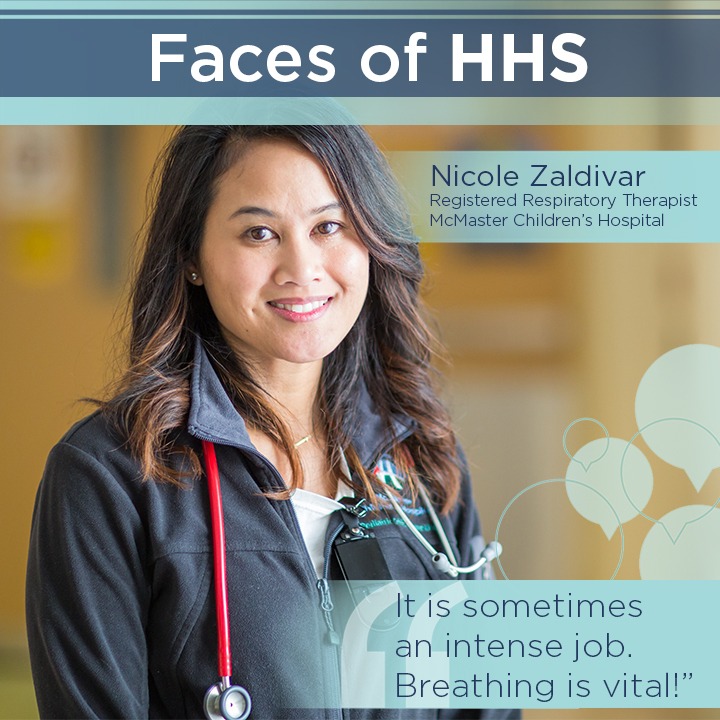
Introducing… a registered respiratory therapist
Nicole Zaldivar is a registered respiratory therapist (RRT) at McMaster Children’s Hospital (MCH), in the Pediatric Intensive Care Unit (PICU) and Pediatric Emergency Department (PED). She has worked at Hamilton Health Sciences for 10 years.
Favourite colour: red/ book: The Alchemist, Paolo Coelho/ vacation spot: the beach/ music: anything positive and upbeat/ animal: puppies/ food: a good burger
“I often try to explain my job by explaining some of the things that I do. Like, initiating and maintaining life support and respirators, or taking over a patient’s breathing while they’re being stabilized.”
When you tell people what you do how do they usually react? I always get: “Wow, that sounds intense!” from non-health care people. It sometimes is an intense job, as breathing is vital! Respiratory therapists provide advanced life support to the sickest patients.
I often try to explain my job by explaining some of the things that I do. Like, initiating and maintaining life support and respirators, or taking over a patient’s breathing while they’re being stabilized. I can also be making sure asthmatic or emphysematic patients understand how to take their puffers at home, or working in a Pulmonary Function lab performing tests to assess a patient’s lung function.
Tell us about your first day. My first day was actually at Hamilton General Hospital and it was extremely intimidating! It was also my first day working as an RRT, so I was very nervous and a little bit scared. I remember it being quite busy – something I later learned was the norm for the Intensive Care Unit (ICU). Eventually that nervousness went away and always being busy was completely normal.
What do you do after work to unwind? I like to watch sports, either live or on TV. I also enjoy catching up on all my favorite shows. On the weekends I try to spend as much time as I can with my family and friends, trying out new restaurants and travelling.
What made you enter your field of work? I was always interested in science in school, but I wanted a career where I could also help and interact with people. When looking at different careers, respiratory therapy seemed like a natural fit.
“Experiencing the death of a child was a first for me. It’s something I think will always be a challenge working in pediatrics.”
What does a typical day in the PED look like for you? I take a report and then take a look at the tracker in PED. From here, I can see which patients might need respiratory support. I look over their charts and their history and try to determine what brought that patient to the hospital. Then, I go have a look at the patient and perform my assessment. From here, I make recommendations to their team as to what the best treatment plan is for that patient. I work with their team to either facilitate a transfer to another department within the hospital or a discharge home.
As part of the Code Blue team we respond and are ready to provide advanced CPR. So, on some days I am called to answer a Code Blue and focus my efforts there. Sometimes, a trauma has happened and my team and I must help stabilize a patient for their cardiopulmonary needs. Needless to say, I am always busy working behind the scenes and I must be ready for whatever comes through the door!

Describe one of your most challenging days at work. My most difficult day was shortly after I began working at MCH. I had a young patient pass away during a Code Blue, which means the patient was experiencing cardiac arrest (technically a Code Pink in this case). This particular patient was 4 years old and was born with a cardiac abnormality. Over time, this condition caused her to have labored breathing which put increased stress on the heart. Experiencing the death of a child was a first for me. It’s something I think will always be a challenge working in pediatrics.
What is something you wish patients and colleagues knew about you? I hope they know that I’m pretty approachable. You can ask me anything.
“I wish I had more time to get to know our patients. Sometimes my workload can be so heavy that I don’t get to know them or interact with them as much as I would like to.”
Do you have a best friend/confidant at HHS? Yes – her name is Alison Nykolaychuk and she has been an RRT for 20+ years. She currently works as an educator for staff and new respiratory therapy hires at MCH. She’s also an educator for Respiratory Therapy programs at Conestoga College and Fanshawe College. She is very well respected in the RT community and has an open door policy and will always respond any time someone needs help or needs an answer to a question. I love how she always makes you feel like you are a valued member of the team.
What do you wish you had more time for at work? I wish I had more time to get to know our patients. Sometimes my workload can be so heavy that I don’t get to know them or interact with them as much as I would like to.

