Promoting sleep to improve recovery
“Get lots of rest!” When you’re sick, it’s a common phrase to hear from friends and family, along with health care professionals. But sleep plays an even greater role in recovery than you may think.
Why is sleep so important in the PICU?
Poor quality of sleep is a significant contributor to delirium, which can occur in 10-30 per cent of critically ill children. Delirium is an imbalance of chemicals in the brain caused by severe illness and other factors. It leads to confusion, and serious long term changes in mental processing and behaviour.
The Pediatric Intensive Care Unit (PICU) at McMaster Children’s Hospital (MCH) is working on strategies to help prevent and treat delirium, and maintaining healthy sleep-wake cycles is a large part of that.
“Delirium is harmful – it not only leads to longer stays in the PICU, it can cause traumatic and lasting changes to the developing brain.”
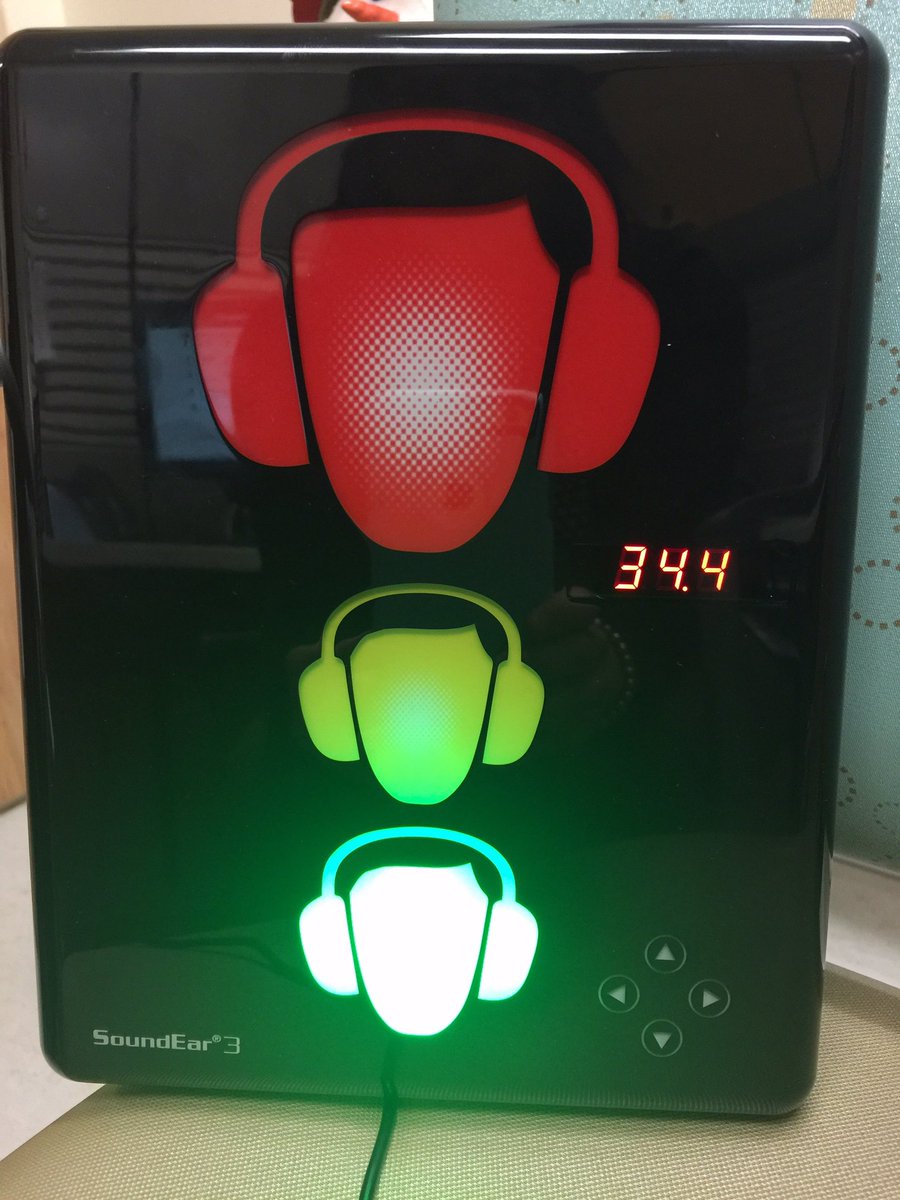
“There are things we can do to prevent delirium, by controlling both medication and the environment,” says Filomena Canci Tavares, clinical leader in the PICU. “Surprisingly, the one of the most effective is strategies is to modify the environment, which include sleep promotion, daytime activity and noise reduction.”
Sleep disruption can cause children to lose muscle endurance, require more time on a ventilator, and have a slower recovery. It also makes a hospital stay less pleasant for patients and their families. Noise, excessive light and being woken up frequently with direct clinical care are the biggest contributors to sleep disruption in intensive care units. To promote healthy sleep patterns and reduce delirium, the PICU at MCH is attempting to control all of these factors as much as possible.
“Delirium is harmful – it not only leads to longer stays in the PICU, it can cause traumatic and lasting changes to the developing brain,” says Dr. Karen Choong, a pediatric intensive care doctor at MCH. “By improving quality of sleep in our patients, we’re reducing the risk for these negative outcomes, and optimizing their recovery.”
Creating a routine to improve sleep
The whole care team in the PICU is involved in creating a daytime routine that will make it easier for a patient to sleep at night. The lights are kept on, and blinds are opened, sedative medications are reduced as much as possible, and movement and physical rehabilitation begin early in the patient’s treatment plan.
“Not only do these strategies help prevent delirium, they make the intensive care unit feel more comforting to help promote healing. Creating that routine is really important to overall recovery.”
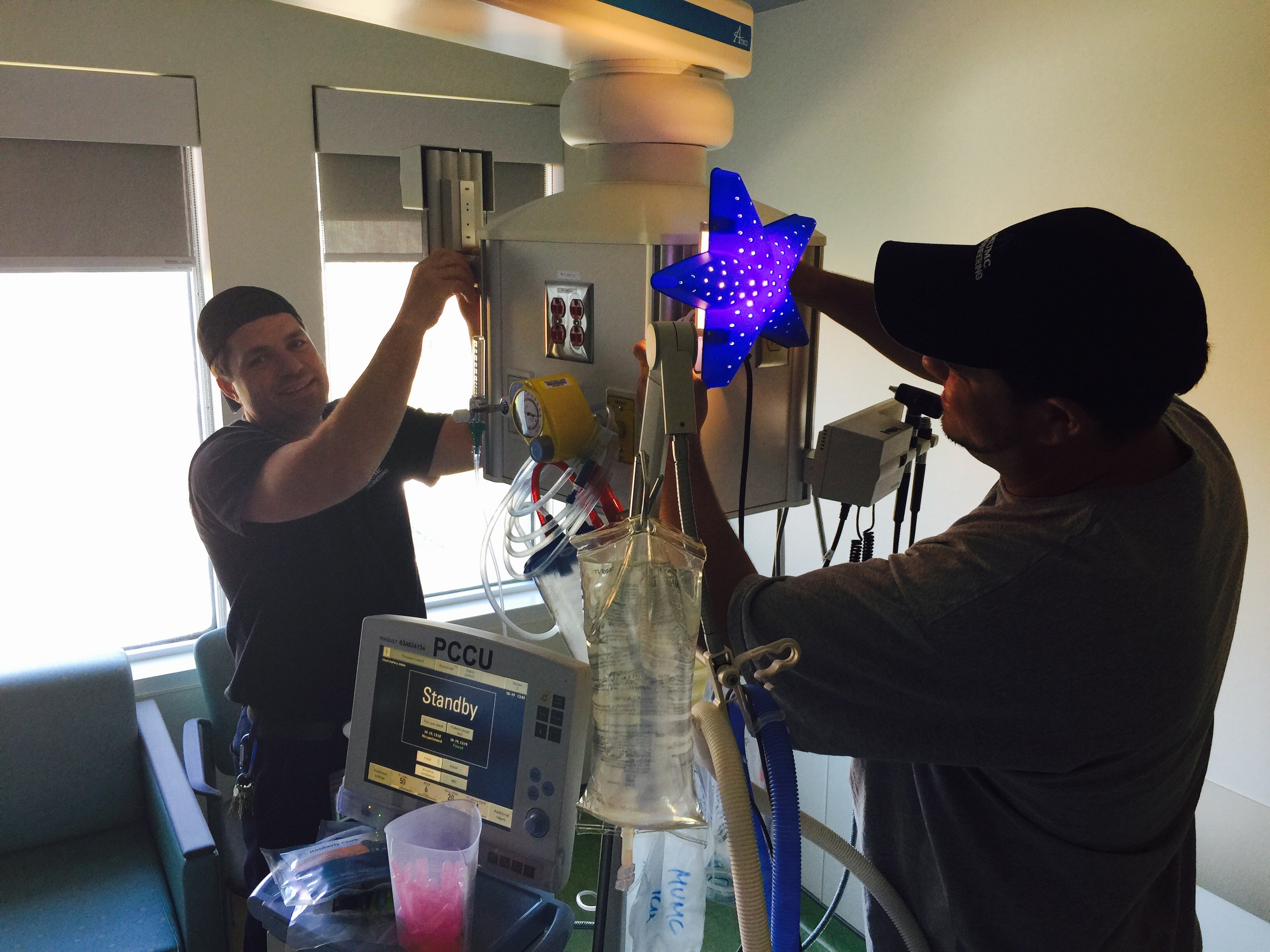
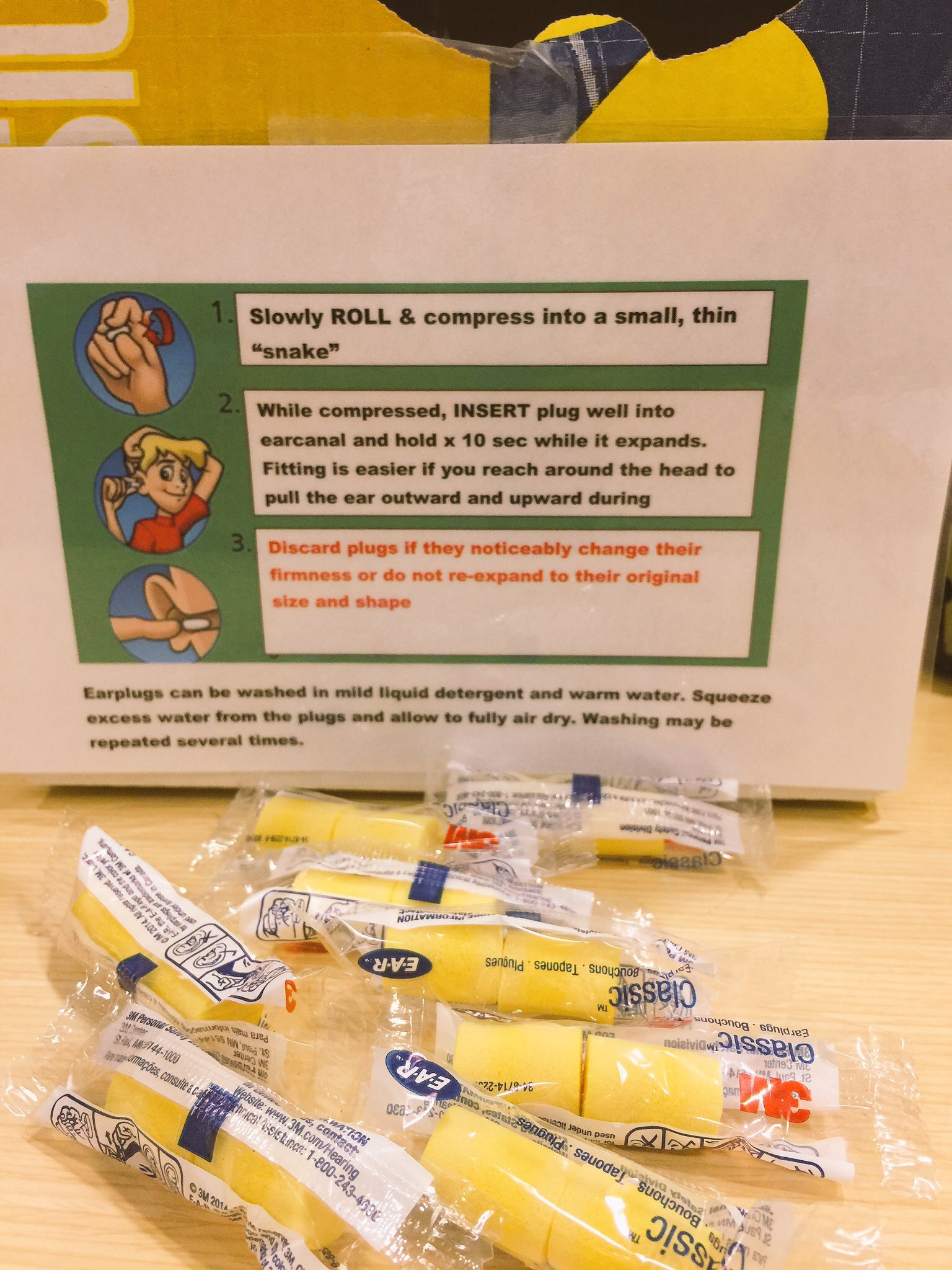
In the evening, the PICU promotes a nighttime routine: lights are out between 10pm and 6am, and the unit becomes a quiet zone. Televisions are turned off, visitors are limited, and elements of the child’s usual bedtime routine, like a bath and story time, are incorporated into care. Each child has a special nightlight in their room and is offered earplugs to further reduce noise. To minimize unnecessary disruptions, the care team clusters tasks together during the night.
Sleep promotion is a collaboration between all care providers, and families are encouraged to get involved as well. Information about delirium is posted around the unit, and they are welcomed to take part in a bedtime routine that will help their child get to sleep.
Measuring success
“We’ve had a really positive response to these improvements, both from staff and families,” says Canci Tavares. “Not only do these strategies help prevent delirium, they make the intensive care unit feel more comforting to help promote healing. Creating that routine is really important to overall recovery.”
To help the children adjust to daylight saving time, team members will work with families to create slight changes to bedtime routines and daytime scheduling to ensure overnight sleep is restful and optimized.
To help improve how they care for patients, the PICU team is actively researching how early mobilization, delirium prevention and sleep optimization can affect a critically ill child and their recovery.