Introducing… a transport nurse
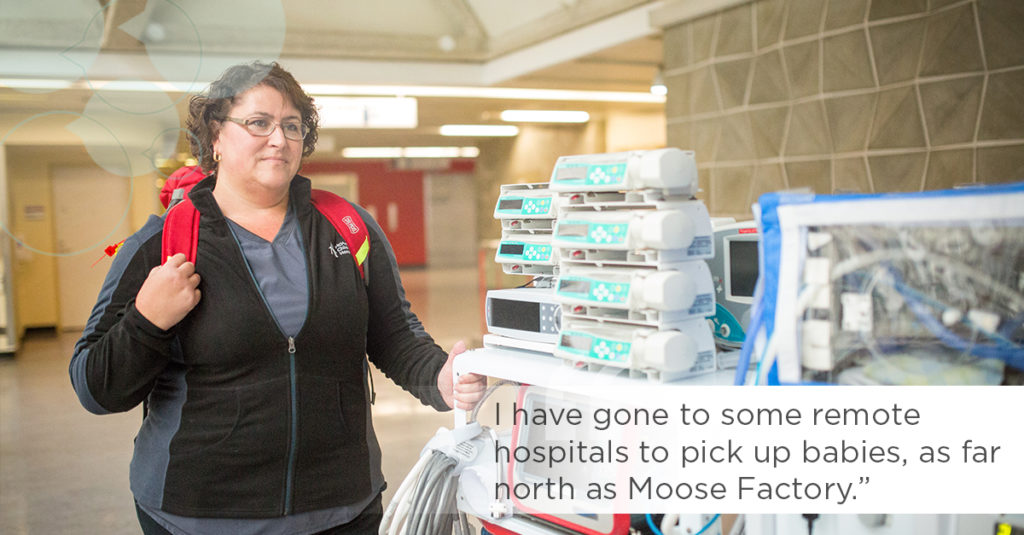
Rene-Ann Hemmings is a neonatal transport nurse at McMaster Children’s Hospital (MCH). She has worked in the neonatal intensive care unit (NICU) for 27 years and has been on the transport team for nearly half that period.
There is an extensive training process that includes skills labs, supervision of these skills in the unit and out on calls, tests and objective structured clinical examinations. It can take up to a year to become certified in this role.
What do you love most about your role?
What I love most is when the care I provide makes a direct difference in the outcome of a baby. It is rewarding to see babies graduate from our unit healthy and happy. Knowing that I played a small role is a great feeling. I also love the leadership aspect of this role. Being an advocate for my patients, giving them a voice when they don’t have one and to provide them with safe and appropriate care is part of why I love my job.
What do you find challenging?
What can be the most challenging part of the role is meeting parents on what they may feel is the worst day of their lives. Their baby may be very sick. It is my responsibility to try to alleviate their fears and develop trust in a short period of time. Sometimes it may mean telling them some difficult news, such as when a baby may pass away before we can transfer them, but thankfully this doesn’t happen often.
I am responsible for stabilizing and transferring babies from hospitals within and outside our region to the appropriate care facility for that infant.
Describe a typical day
MCH is the referral centre for up to 500 transport calls a year. When there is a call requiring a transfer, my partner and I are responsible for stabilizing and transferring babies from hospitals within and outside our region to the appropriate care facility for that infant. We are governed by medical directives that allow us to do medically sanctioned acts such as intubation and ventilation, insertion of umbilical lines and chest drains when deemed necessary to safely transfer some of the sickest babies to our unit. We are essentially the eyes and ears for our doctors who are giving us advice over the phone. It is a huge responsibility and I am proud to be part of this small group of knowledgeable and skilled transport nurses.
When not out on a call, I have several different tasks. This includes helping with deliveries or transporting ventilated babies within the hospital for lifesaving surgery in addition to ordering transport supplies or inputting data.
Tell us about your most gratifying experience at HHS
One of the most rewarding experiences happened when my partner and I needed to get to a hospital as quickly as possible. An Ontario Provincial Police (OPP) officer was gracious enough to give us a ride as we were urgently trying to get to a sick baby with a collapsed lung. He needed a chest drain and there was no one in that hospital that was comfortable doing the procedure. After the procedure, he was still unstable. After a few hours of other procedures to stabilize him, we could finally transfer him safely to MCH. The baby’s mother contacted me months later to tell me how amazing her little boy was doing and it was in part because of that day. When we have stressful days I remember how good it feels to have these successes.
What’s one thing people would be surprised to learn about your role?
One of the things they may not know is how often I visit some remote hospitals to pick up babies. I’ve been as far north as Moose Factory, Ontario, as far northwest as Thunder Bay and as far east as Ottawa. I fly in Ornge helicopters and fixed wing airplanes, as well as ride in ambulances and private transfer vehicles (and the occasional OPP vehicle) to get where we need to go. My shift may finish at 7:30 but it is not unusual to go past that. Thankfully I have a supportive family at home who may not see me until much later than expected.
