Reducing the impact of COVID-19 on chronic illnesses – a growing challenge
 By Dr. Sara Ahmed
By Dr. Sara Ahmed
For over a year now, healthcare professionals have been at the forefront of this crisis – working day and night to deliver the best possible care to patients in hospital and in community settings.
Long-lasting impact
While COVID-19 has pushed hospital systems to the brink, family physicians and specialists working in the ambulatory environment also rose to the challenge. They improvised and adapted to the world of virtual medicine to stay in touch with patients and maintain their continuity of care. Unfortunately, despite these efforts, access to health care, patient hesitancy, and lapses in follow-up persist. This disruption of care may have a long-lasting impact on chronic health outcomes that will likely surpass the duration of the COVID-19 pandemic.
Despite the pandemic, cancer, heart attacks, stroke and diabetic complications remain life-altering and life-threatening conditions
Since March 2020, isolation measures to decrease the risk of COVID-19 exposure and spread have been widely implemented in health institutions. Although a necessity of the time, these measures have had an impact on elective and non-emergent services. Ambulatory care physicians have been challenged with prioritizing the provision of care to patients through telemedicine. This, augmented with the fear of contracting COVID-19, has deterred patients from seeking in-person care in a time-sensitive manner. As a result, many chronic medical conditions may have gone undiagnosed and unmonitored.
Increasing complications in chronic illnesses
While the full extent of the impact of COVID-19 on individuals with chronic illness may take time to fully understand, anecdotally, it has been reported that we are already seeing a rise in complications secondary to poorly controlled diabetes, kidney disease and cardiovascular disease. Similarly, we are also seeing more patients presenting with advanced stages of cancer – lung cancer being the most aggressive.
Reduced patient volumes and implementation of staggered visits to minimize COVID-19 exposure has created a backlog of patients who are waiting for their screening and surveillance testing. Hence, there is a growing concern that we may end up detecting cancers at a much later stage where treatment options will be limited and prognosis poor.
Keep your appointments
It has been a year since COVID-19 was declared a pandemic. We have come a long way and have learned how to safely provide medical care during such unprecedented times. With the majority of ambulatory procedures returning to pre-pandemic levels, we must maximize our efforts to reach out to patients with chronic illnesses. It is critical to raise awareness about the harrowing consequences of not seeking care in a timely manner.
Despite the pandemic, cancer, heart attacks, stroke and diabetic complications remain life-altering and life-threatening conditions, so it is crucial to keep appointments for screening tests and follow-ups. Early diagnosis and treatment can make all the difference.
Here for vulnerable patients
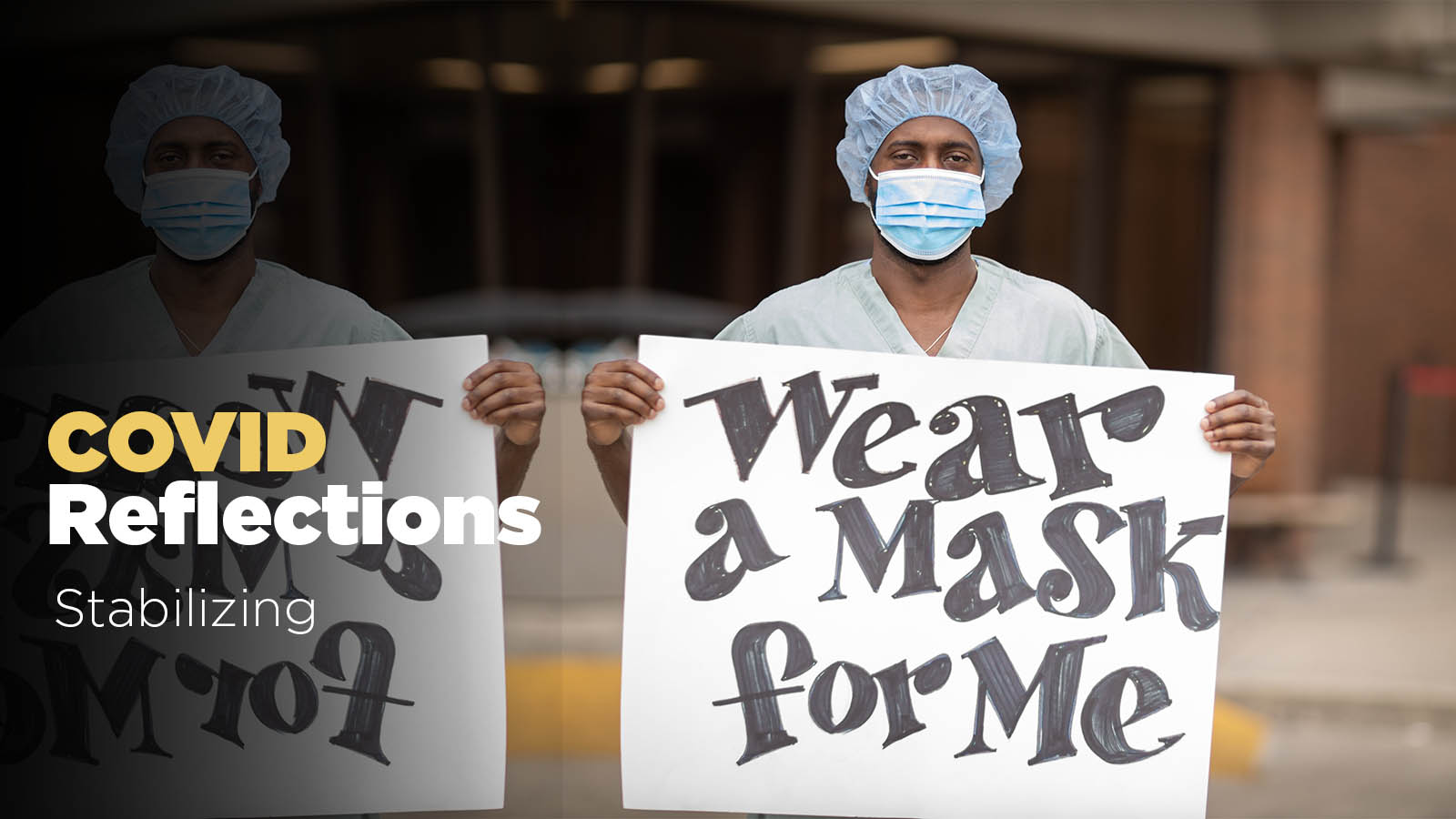
Similarly, it’s important to reassure patients that our hospitals have proactively instituted measures to ensure the safety of in-person care. Screening at entrances, strict masking, physical distancing, and enhanced cleaning are all part of the protocols.
With vaccine distribution, we have begun to see the light at the end of the tunnel. It is about time we start focusing on the optimization of routine care delivery in ambulatory settings. Hopefully this way, we can curtail the detrimental impact of delayed care on health outcomes for vulnerable patient groups.