COVID Reflections: The beginning
March 11 marked the passage of one year since the World Health Organization declared a global pandemic for COVID-19. HHS is commemorating this time by acknowledging the heroic efforts and achievements of our workforce in response to this pandemic. We also recognize the challenges, loss and grief of this past year and extend our deepest condolences to those who have lost loved ones during this time.
These stories highlight milestones over the past year in our organization’s fight against the disease and for our community. This is chapter 1 of 4.
The beginning
The start of March 2020 brought the promise of better weather, March Break for kids, St. Patrick’s Day celebrations and sunny times ahead.
But the world had something else in store for us.
On March 11, 2020, the World Health Organization declared a worldwide pandemic of a virus called “COVID-19” – a term we know all too well more than one year later.
On the same day the pandemic was declared, a Hamilton Health Sciences (HHS) physician was identified as the first COVID-19 case in our region. This was the start of what would become known as the pandemic’s “first wave” and brought the virus right to our doorstep.
Rewind to January 2020 to see that HHS was already gearing up and preparing an action plan. After the country’s first case was confirmed here in Ontario, the hospital began sharing information about the coronavirus with staff and working closely with infection prevention and control team members that continue their critical role as the pandemic persists and grows even today.
In the first few days and weeks of the pandemic landing locally, HHS worked to keep our community safe by opening COVID-19 testing centres and laboratory support, adding screening to our hospital entrances, creating a specialized COVID unit at the Hamilton General Hospital to care for COVID positive patients, hunting down personal protective equipment from around the globe, and overall reacting with lightning speed to put infection protocols into place throughout the organization.
All the while, staff and physicians dealt with constant questions about their own safety, how to balance family needs with children out of school, and the best way to transition of a portion of HHS staff to work from home.
COVID-19 Assessment Centre opens
On March 16, just days after the WHO announcement, HHS and our partners opened a COVID-19 Assessment Centre at HHS’ West End Clinic to test people for the virus by appointment. The centre was one of two opened in the city (a third was added later).
The clinic was a joint effort by Hamilton Health Sciences, St. Joseph’s Healthcare Hamilton (SJHH), Public Health Services, primary care physicians and the Ontario Ministry of Health to help safeguard and support the health and wellbeing of people in our community.
“Thank you to everyone working tirelessly at these centres to help contain the spread of COVID-19 in our community,” says Lucas Milinovich, director of urgent and ambulatory care.
Screening at designated entrances
Another effort to stop the spread of the virus that continues a year later is the screening process for anyone entering HHS sites.
Before March 2020, anyone could walk into any HHS location without waiting in line, answering screening questions, using hand sanitizer, and being asked to wear a medical mask. But times have changed.
Since then, HHS screeners have been the first faces patients and staff see when stepping inside an HHS hospital or healthcare centre. Whether pre-screening electronically from home or answer screening questions at the desk, the screening process is vital to limiting the spread of COVID-19 at our facilities.
“I’m grateful for this opportunity to express my thanks and recognize the important work that has been done by our HHS screeners over the past year,” says Nancy Hayes, manager of volunteer resources and multi-site screening. “As the first point of contact for many entering our sites, their perseverance and dedication to ensuring this critical step is completed has protected us all from the spread of this virus. Thank you for all you have done to keep our hospitals safe.”
At the same time screening became mandatory at all entrances, HHS made the tough decision to stop most visitors from entering our buildings. This lasted for a period of several months.
Lab operates around the clock
COVID tests from the assessment centres are processed at the lab, yet another program vital to tracking the course of the virus.
As the pandemic picked up speed in wave one, the Hamilton Regional Laboratory Medicine Program (HRLMP) started operating around the clock to test COVID-19 samples from hospitals in Hamilton, Burlington, Niagara, Kitchener-Waterloo, Cambridge, Guelph, Markham, Uxbridge, and many more locations across southern Ontario. HRLMP is a joint program of HHS and SJHH.
“It’s very fast-paced,” says technical specialist Candy Rutherford, who has worked for HHS for more than 45 years. The team’s focus is on getting their job done right, and then fast.
Before the testing could even start, there was an incredible amount of work just to get ready, including validating materials, designing tests, and just as importantly, planning for worker safety.
“We went live on March 16, 2020, processing about 200 COVID-19 tests per day. We continued to innovate with new robotics to get to our current capacity of 4000 tests per day,” says Dr. Marek Smieja, Interim Chief of Laboratory Medicine at HRLMP. “We have completed nearly half a million tests in the last year. Our team’s hard work and dedication is crucial to the COVID-19 effort not only in Hamilton, but in the region.”
Designated COVID unit at Hamilton General Hospital
On March 20, 2020, the first HHS patient requiring hospital care for COVID-19 was admitted to Hamilton General Hospital’s 8 West – a unit that officially became the designated location for COVID patients at HHS ten days later.
“When we got our first COVID-19 admission, there was fear of the unknown,” says Dale Bialas, manager of the initial COVID unit on 8 West. “Nevertheless, the team was determined to show up and care for our patients.”
As COVID-19 spread in the community, Hamilton hospitals recognized the need to consolidate COVID care and expertise in fewer, select locations. HGH’s 8 West became the spot. When the 8 West team realized they were ready for others to share the responsibility, the COVID unit transitioned to another location at HGH, 5 West. Eventually in January of 2021, HHS opened a second COVID unit at Juravinski Hospital.
Nearly 30 residents from the Rosslyn retirement residence were urgently transferred to the COVID unit in May, which was the largest admission in under 24 hours. More than 60 of the home’s 66 residents were admitted to HHS or SJHH when it was evacuated because of an outbreak.
Managing COVID units in the hospital has been a collaborative effort, says internal medicine physician Dr. Mohamed Panju.
“One of the silver linings of COVID was the increase in team work,” he says. “Clinically, patients needed a team of healthcare providers which include nursing, occupational and physical therapy, social workers, pharmacy and respiratory therapists working with the physicians. Administratively, the infection control team was very important with regards to communicating with public health and clinical units. The educators and were another important group which provided front line teams with proper PPE technique. COVID care in hospital was looked at from a regional perspective and the communication between and frontline workers and administration was extremely important.”
A hunt for personal protective equipment
As the COVID-19 pandemic spread worldwide, sourcing and storing large amounts of personal protective equipment (PPE) became a critical challenge for many healthcare providers across the country – and HHS was no exception.
A multi-disciplinary team of about 15 people was pulled together quickly with representation from Health Safety & Wellness, Infection Control, Procurement, Supply Chain & Logistics, Clinical Education, and Quality. The team helped to assess and process external offers of PPE, equipment and other supplies, such as cleaning supplies and sanitizer.
“We were doing everything we could to source innovative solutions and get this equipment into the hands of our staff and doctors. We were working faster and smarter than we ever have to access the PPE we need in new and different ways,” says Bryan Herechuk, quality and value improvement program interim director.
“This was a unique opportunity to work collaboratively with non-traditional partners in local industry in the Hamilton area in order to meet a critical PPE shortage through innovative and rapidly developed solutions, working together to deliver in days or weeks what would normally take months or years.”
Partnerships like these were so important in a time of need.
The volume of PPE required to meet the needs of staff, physicians, patients and visitors exceeded the regular storage space available on site.
“Hospitals typically store pandemic supplies in an offsite warehouse for events like COVID-19,” says Annette LaCivita, manager of supply chain logistics at HHS. “The impact COVID-19 had on our supply chain meant we had to look further for supplies and purchase larger volumes to meet the expected demand.”
HHS sourced a temporary warehouse with approximately 20,000 sq. ft. of storage space.
While a few challenges remain, our PPE supply is stable and the temporary warehouse will close this month as HHS transitions to a new inventory storage model.
Infection Prevention and Control
The Infection Prevention and Control (IPAC) team was first engaged in COVID-19 work in January 2020, after the Wuhan Municipal Health Commission in China reported a cluster of cases of pneumonia in Wuhan.
“The IPAC team was essential in developing information for frontline staff on how to test, flag in IT systems, and screen patients, staff and visitors for COVID risk factors to prevent hospital-acquired cases and outbreaks,” says Dr. Sarah Khan, infectious diseases specialist at HHS. “We had to rapidly act upon dynamically changing public health recommendations for the prevention and control of hospital infections, and work closely with occupational health, microbiology, clinical practice and education, patient experience, and public health to keep patients and staff safe and informed on best practices.”
IPAC was critical in the creation of the PPE Task Force, Perioperative and Procedural Guidance, visitor guidance, informing policy at the subject matter expert committee, and patient flow at each site’s incident management command tables. The team continues to provide guidance for patient care, research and educational policies to keep our staff and patients following best practices based on the evolving evidence about COVID-19.
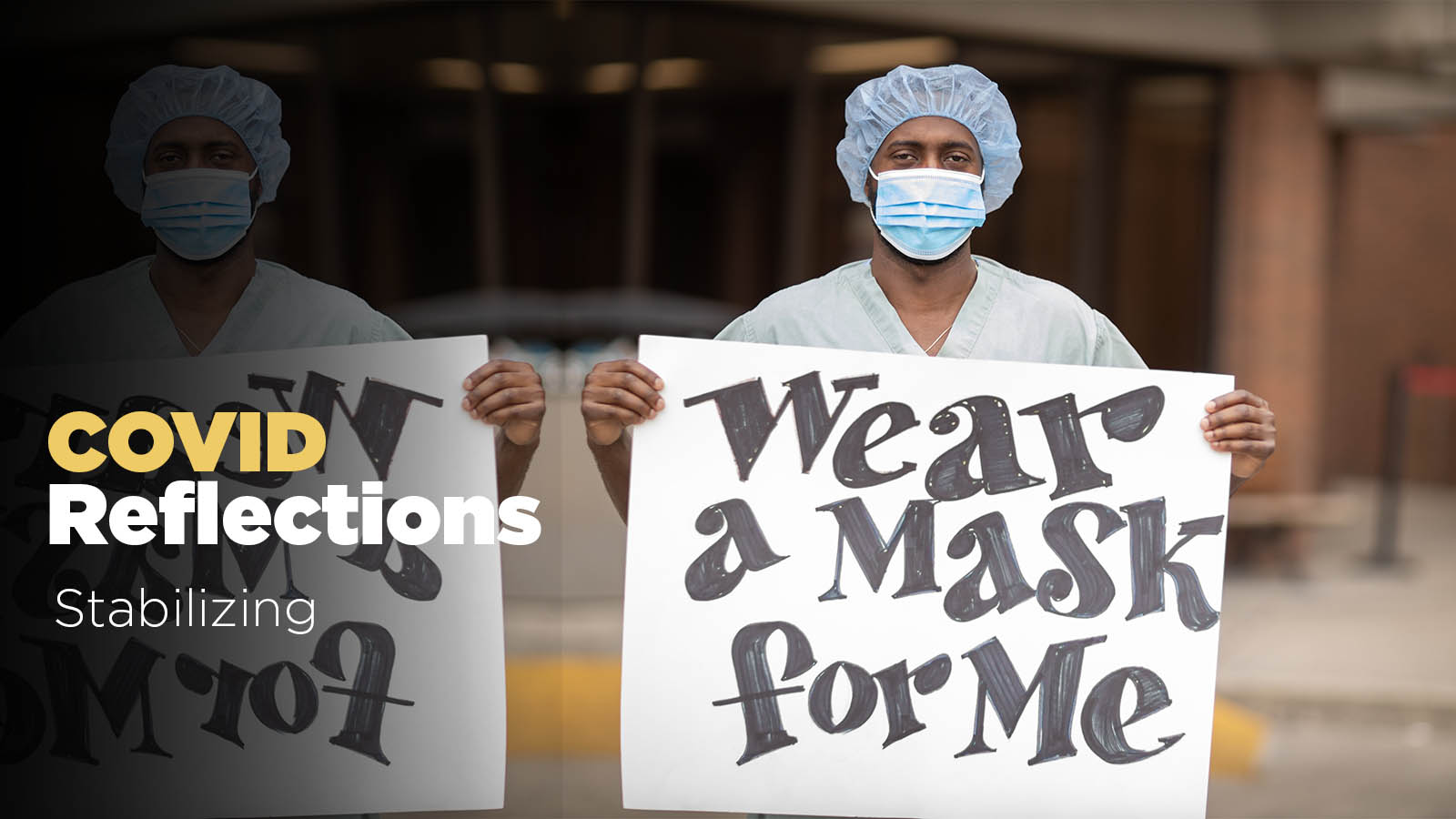
Messages of hope
As the pandemic started to take a toll, the community stepped up to support frontline workers with messages to support displayed on home windows, written in sidewalk chalk, or painted on rocks. HHS launched our #signuptosupport campaign to encourage the community to continue to show gratitude to our frontline workers.
Gradually, the first wave crested, and then case numbers decreased. As the summer approached, HHS staff and physicians began to experience some stability after a turbulent start of the pandemic.
Read chapters 2-4.