“When you can’t breathe, nothing else matters.” Respiratory therapists are vital to COVID care
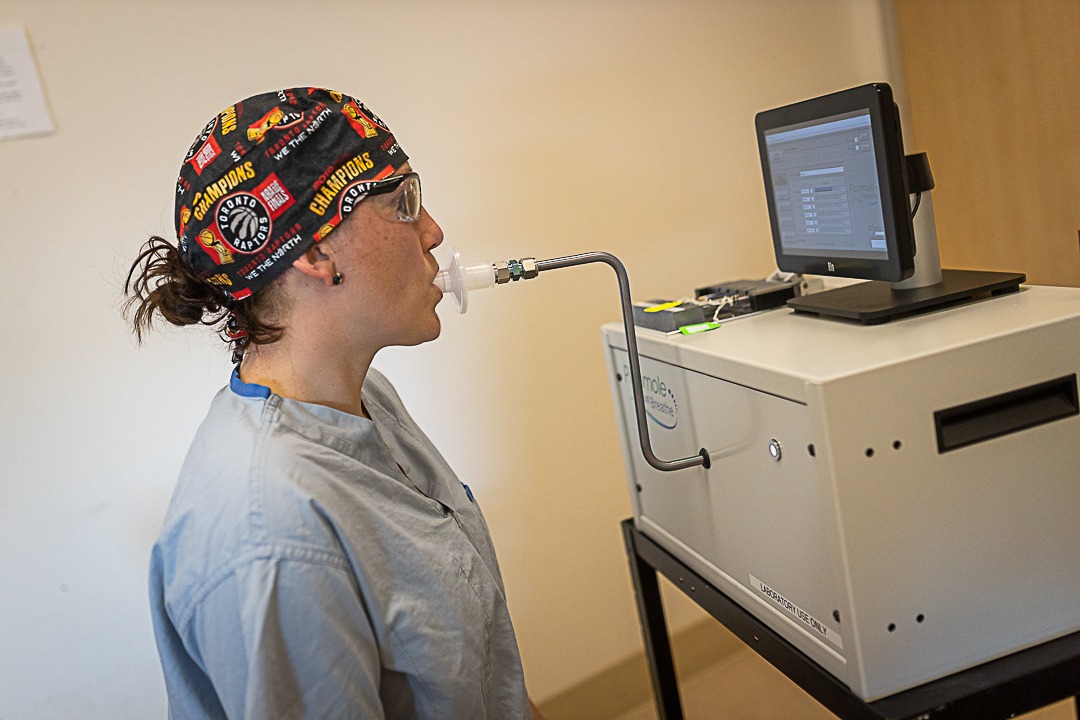
“We see patients when they are at their very worst,” says respiratory therapist (RT) Ally Ruzycki-Chadwick. Her job is to help patients who have trouble breathing. The role of RTs is critical – especially when fighting a respiratory infection that attacks the lungs like COVID-19.
“When you can’t breathe, nothing else matters,” she says.
The role of an RT
Ruzycki-Chadwick rotates between units at Hamilton Health Sciences’ (HHS) Hamilton General Hospital (HGH). Depending on where she is needed, she will float between the intensive care unit (ICU); emergency department; hyperbaric unit, which provides oxygen therapy; the Rapid Assessment of Critical Events (RACE) team, which provides critical care to people outside of the ICU; as well as throughout the hospital’s different wards.
Respiratory therapists assess and monitor patients who are having difficulty breathing. They help determine the appropriate treatment options and therapies, from giving medication and applying oxygen to inserting breathing tubes and managing the ventilators that help keep people breathing when they can’t on their own.
During the pandemic, Ruzycki-Chadwick and her colleagues have been working with COVID-positive patients on the COVID units and in the ICU.
Ventilator management
Patients on the COVID units are able to breathe on their own or may need some assistance, such as oxygen.
On the other hand, the majority of patients in the COVID ICU require a ventilator to breathe. This piece of equipment can be programmed to breathe for patients who are are not able to breathe on their own. The process requires intubation, where a tube gets inserted through the mouth and into the airway.
RTs program ventilators to deliver oxygen throughout the body and expel carbon dioxide, and also to keep breathing muscles engaged or retrain those muscles that have been weakened. Sometimes the “weaning” process from the ventilator can be a long one.
“There are lots of numbers that we monitor to see how efficiently we can offset the disease process from the lungs,” says Ruzycki-Chadwick.
A ventilator doesn’t cure COVID-19 or other illnesses, but it does give the body time to heal.
Adapting to a challenging landscape
Ruzycki-Chadwick has worked at HGH for nearly 19 years. She says the COVID-19 pandemic has brought her profession to the forefront.
“The teamwork is astounding. We’re all in this together.”
There are about 150 RTs at HHS and 3,500 in Ontario. The COVID-19 pandemic has caused them to adapt to a changing and challenging landscape.
“We have adapted, we have researched, and we have expanded our knowledge. We have leaned on our colleagues throughout Ontario, Canada, and the world to see what others are doing. It’s been a huge learning curve through all of this,” she says.
“But what has shone through is that our team has really stepped up to the plate. The teamwork is astounding. We’re all in this together.”
On top of performing duties where people’s lives are at stake, they are working in full personal protective equipment (PPE) to protect themselves from the virus, which makes the work even more challenging.
Balancing work and home life
In addition to her full-time job, Ruzycki-Chadwick is the president of the College of Respiratory Therapists of Ontario, she provides training to smaller hospitals, and is a mom to three children navigating constant changes to their education.
“It’s been a bit of a balance,” she says. “My husband and parents have really supported me so I can be in the hospital.”
She anticipates the third wave of the pandemic will be the most trying to date. While it’s overwhelming to think about, she knows her work family and her home family have her back.
“They are my crutch.”