HHS physicians lead study to test COVID-19 breath screening technology
Two Hamilton Health Sciences (HHS) physicians are leading a McMaster University research project with Canadian medical device company Picomole Inc. to test breath screening technology developed to detect COVID-19 in patients.
The study is being led by Drs. MyLinh Duong and Tim O’Shea. Duong is an HHS respirologist and an associate professor in McMaster’s department of medicine. O’Shea is an infectious diseases and internal medicine specialist at the HHS Juravinski Hospital and an associate professor in the division of infectious diseases at McMaster.
The six-month study will collect breath samples from 100 COVID-positive patients as well as 100 non-COVID patients for the control group at three sites: Juravinski Hospital, St. Joseph’s Healthcare Hamilton and St. Mary’s General Hospital in Kitchener.
Detecting COVID through breath
 Breath analytics involve the collection, processing, and analysis of breath samples to identify volatile organic compounds associated with specific diseases. Using proprietary breath analytics technology, Picomole is able to generate a fingerprint-like analysis of human breath, which can be used for fast, non-invasive disease detection.
Breath analytics involve the collection, processing, and analysis of breath samples to identify volatile organic compounds associated with specific diseases. Using proprietary breath analytics technology, Picomole is able to generate a fingerprint-like analysis of human breath, which can be used for fast, non-invasive disease detection.
This study is looking to identify compounds in breath that distinguish COVID patients from non-COVID patients. Organic compounds are often associated with environmental issues, such as contributing to certain types of air pollution. But some are naturally occurring in our bodies, as a byproduct of our cells when they undergo metabolism.
“So when cells become abnormal, such as cancerous or infected cells, they metabolize in a different way and their byproducts can be released into the breath which is then expelled with each breath,” says Duong.
Potential to diagnose COVID-19 in a non-invasive way
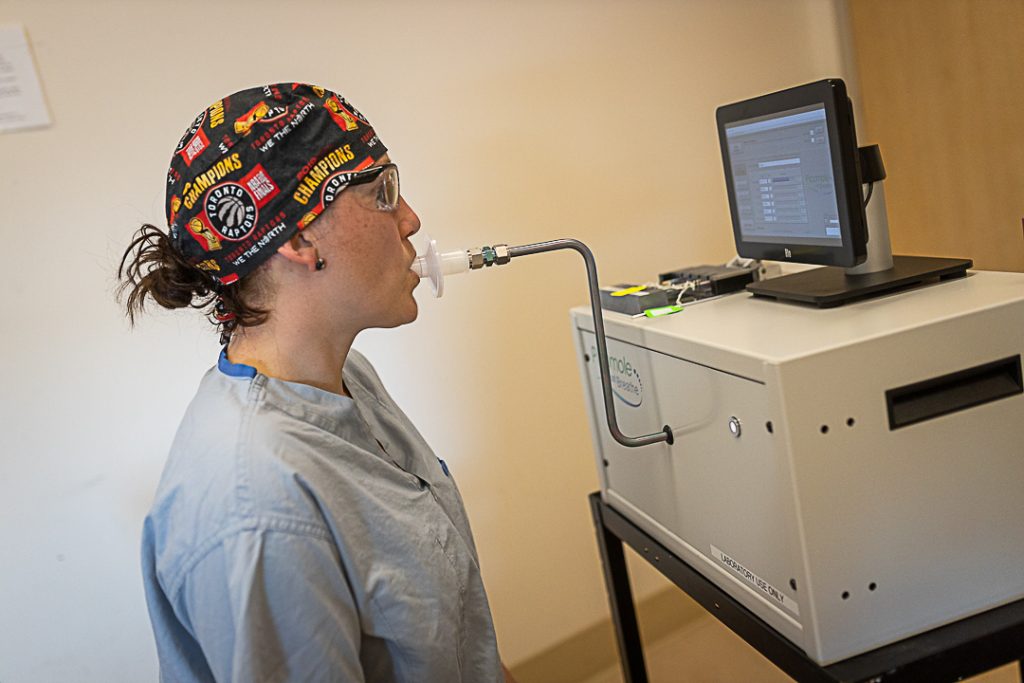
The device used to collect samples is about the size of a countertop microwave oven, and has a mouthpiece that the patient exhales into. Collected breath samples are concentrated in tubes, frozen and sent to Picomole’s laboratory in Moncton, New Brunswick for analysis.
“Our team is excited to partner with McMaster University and Hamilton Health Sciences in this research project to screen for COVID-19 in breath,” says Dr. Stephen Graham, CEO of Picomole. “These are challenging times for many, and Picomole is eager to be involved in the fight against COVID.” Picomole has also been using this technology for studies into detecting lung and breast cancer.
“With a breath test, we can directly collect a sample from inside the lungs without putting patients through an invasive procedure and placing staff at risk of contracting COVID.”
Duong is excited for the potential to diagnose COVID in a non-invasive way that’s safer for healthcare staff.
“Once COVID gets into a patient’s lungs and they develop pneumonia, their nasal swab may become negative since the virus is no longer in the nose or throat,” says Duong. “The only way to confirm they have COVID is through bronchoscopy, where an instrument is inserted into the airways deep inside their lungs to collect samples. This is a high-risk procedure for staff because it causes the patient to cough and generate aerosols which are highly infectious. With a breath test, we can directly collect a sample from inside the lungs without putting patients through an invasive procedure and placing staff at risk of contracting COVID.”
Next steps
If successful, the next phase of the study will look into whether this technology can detect which stage of COVID – from early to late stage – a patient is experiencing based on what is detected in the breath, which may be different during the early stages versus later stages of the infection. The goal will be to develop a rapid test that can quickly detect changes in a COVID patient’s condition.
“We’re hoping to be able to stage people without going through CT scans and chest x-rays for diagnosis,” says Duong. “This would also allow us to diagnose pneumonia and determine COVID staging in the community, without patients coming into the hospital.”
The research project is funded by the Department of National Defense (DND) IDEaS grant.
“Canadian innovators are among the most creative and innovative people in the world, says Canada’s Defence Minister Harjit Singh Sajjan in a prepared statement. “We are all on the same mission to conquer COVID-19 and to keep the members of the Canadian Armed Forces, and all Canadians, safe.”



