Monitoring surgical patients while recovering at home
This spring, when ICU space was limited due to the pandemic, Diana Brozovic required surgery. She had a cancerous tumor attached to the outer wall of her stomach that needed to be removed.
Her surgery at Hamilton Health Sciences’ (HHS) Juravinski Hospital and Cancer Centre (JHCC) went well and thanks to the surgical transitions program, she was discharged a week later to continue her recovery at home.
Connecting by the touch of a screen

Dr. Flavia Kessler Borges
“The surgical transitions program connects patients from the comfort of their homes with their health care team by just the touch of a screen,” says Dr. Flavia Kessler Borges, physician with the surgical transitions program who played a critical role in establishing the monitoring protocol and outlining the situations which would require a physician to be consulted. “The virtual care multidisciplinary team provides the needed support throughout the critical early days of surgical recovery to increase patients’ safety and improve quality of care.”
The program allows patients to recover at home while being remotely monitored by a hospital-to-home virtual care team from the hospital command centre. Patients enrolled in the program are given a Cloud DX Connected Health kit upon discharge. The kit includes a tablet paired with equipment to capture vital signs and weight. The virtual care routine includes daily patient vital signs review, nurse video visits and assessments, surgical wound photography and review, and medication and pain assessments. Together, the nurses and physicians review the patients’ recovery daily.
The surgical transitions program operates seven days a week, 14 hours a day. It helps people go home from the hospital sooner, and decreases the chance they will need to come back. The program also reduces unnecessary trips to the emergency department. Plus, the program identifies and addresses complications that can arise after surgery in a simple and efficient manner.

The a Cloud DX Connected Health kit that is provided to patients in the surgical transitions program.
Identifying complications before they become an emergency
That’s what happened with Brozovic.
About a week after she went home, the team at the command centre was concerned with her blood pressure readings. They called to check on her and she was feeling unwell. So, she was sent for some tests in her home community, about an hour away from Hamilton. When the results were in, the virtual care team instructed her to go to the emergency department at the JHCC.
“Since our program has everything documented on the patients, we were able to connect with the team at the JHCC to ensure they were prepared for Diana when she arrived,” says Mikeera Dobson, a registered nurse with the virtual command centre and Brozovic’s lead nurse.
The issue for Brozovic was a gastrointestinal bleed, which required a small procedure to stop the bleeding. Once she was home, Dobson checked on her every day to ensure no additional complications arose.
“It’s been amazing to see the difference this program has made in our patients’ lives,” says Dobson. “Not only can we catch complications early, like with Diana, but in many cases we can prevent patients from even having to go to the emergency department altogether.”
Brozovic says she couldn’t agree more.

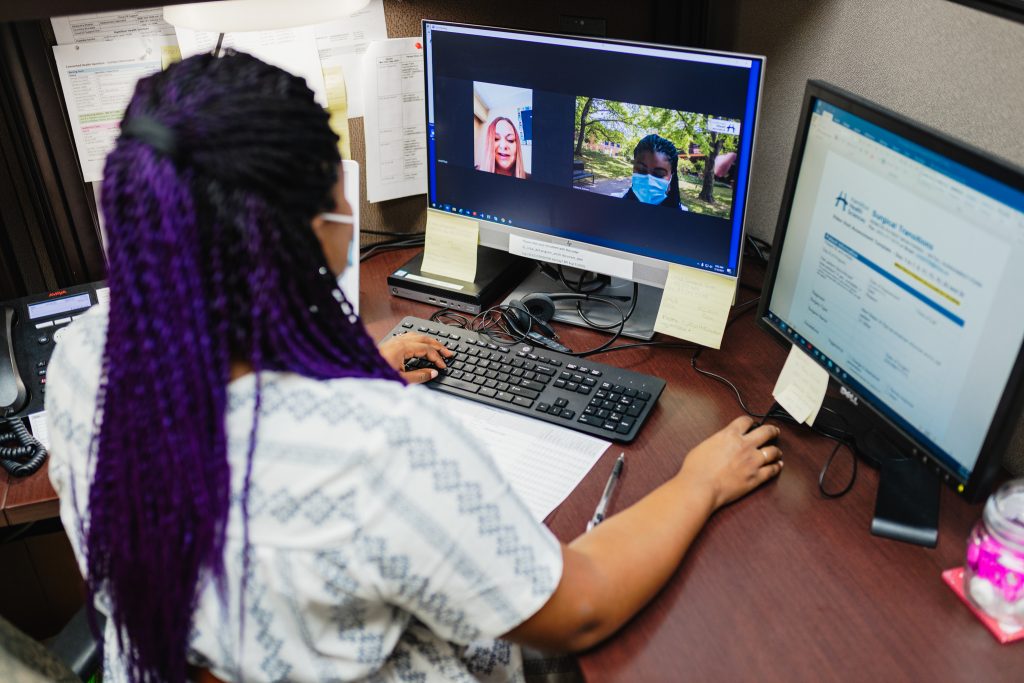
Mikeera Dobson, registered nurse, at the virtual command centre for the surgical transitions program.
“Being part of this program was a huge security blanket for me,” she says. “Having the resources available as well as the support of the medical team was terrific. I could ask questions when I needed to and I even got familiar with vitals. I felt very well cared for and can’t thank the team enough.”
Moving forward
Thanks to provincial funding in early spring of this year, HHS and St. Joseph’s Healthcare Hamilton (SJHH) partnered to provide more surgical patients with the virtual care option of the surgical transitions program. The program is based on the latest Canadian research led by a team of surgical care researchers at the Population Health Research Institute, a joint institute of HHS and McMaster University. It provides an interprofessional team of perioperative physicians, including cardiologists, surgeons, and anesthesiologists, as well as nurses to support virtual rounds and patient care.
As a result of the third wave of the pandemic, both HHS and SJHH have had to postpone thousands of non-urgent procedures. While surgical procedures are currently in the process of ramping back up, the surgical transitions team hopes to help more patients get their surgery sooner, safely.




