“Eating disorders are now part of our history, and not our everyday life,” says mother of teen patient
Mind Over Matter: Inside the Shadow Pandemic of Pediatric Eating Disorders
The pandemic has thrown many young people into crisis. Prolonged periods of social isolation, disconnection from regular routines and in many cases, a new normal for family dynamics is resulting in the growth of increasingly unbalanced, unhealthy, concerning and dangerous habits.
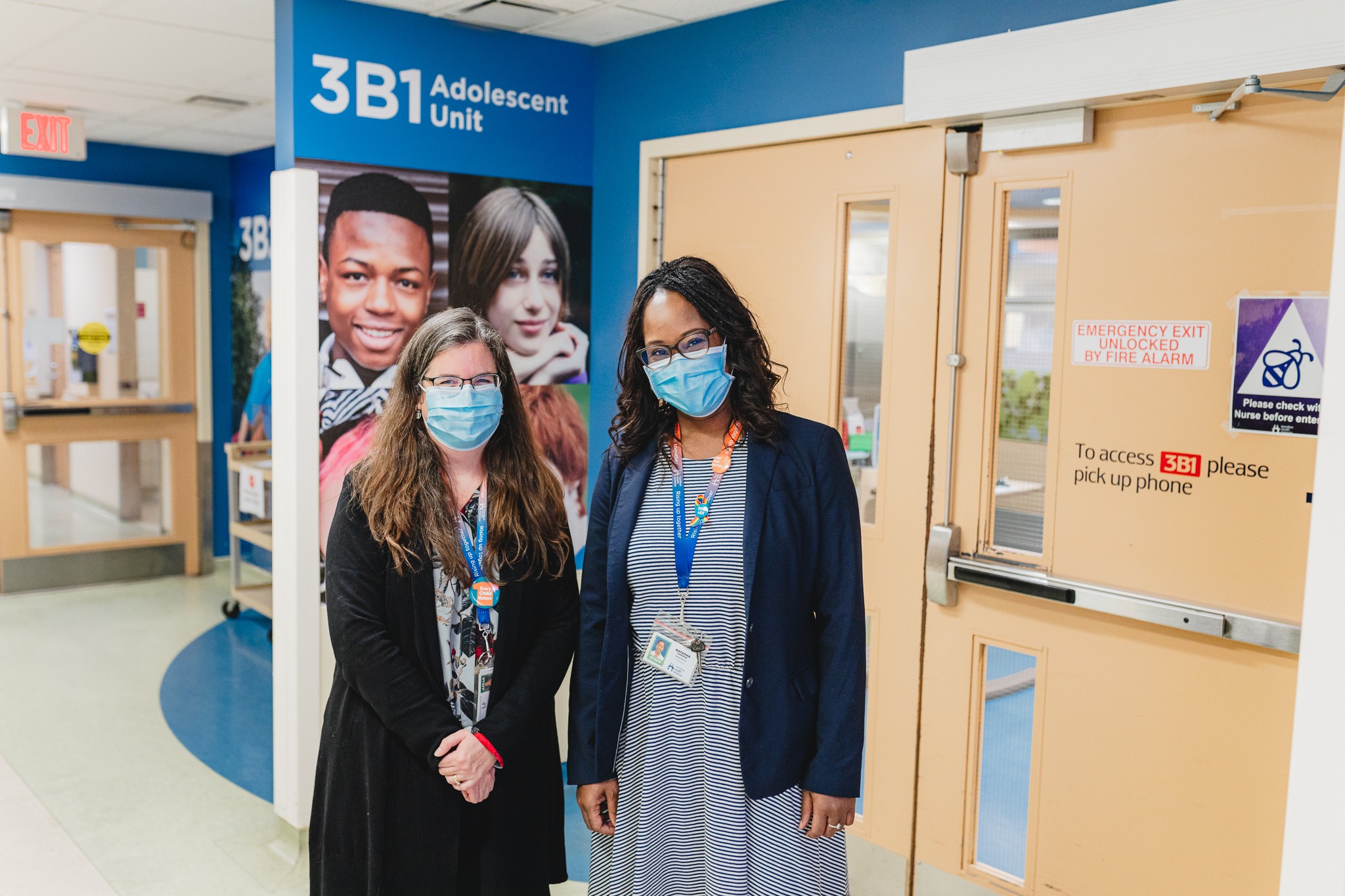
The nationally recognized Pediatric Eating Disorders program at McMaster Children’s Hospital is seeing an unprecedented number of children and youth coming to the hospital with serious mental and physical health concerns; a trend that is anticipated to continue into the future.
This is the second piece in a three-part series shining a light on the eating disorder diagnosis and its treatment from three different and unique perspectives: the provider, the patient and parent, and the program administration.
Part 2: “Eating disorders are now part of our history, and not our everyday life,” says mother of teen patient
It’s possible to get yourself back from an eating disorder, says a 15-year-old patient who accessed care from Hamilton Health Sciences’ McMaster Children’s Hospital’s (MCH) inpatient eating disorders program.
“Don’t wait to get help,” says the patient’s mother, “and trust your gut. Eating disorders are not a life sentence. There is great care available and there is hope.”
The patient and her mother quoted in this piece have asked that their names not be published. However, they both wanted to share their story in the hopes that their message and their family’s journey with an eating disorder diagnosis can help others facing a similar situation.
The journey
The patient’s mom says she could tell her daughter was struggling with an eating disorder. She ate very little and was very strict about her food choices. She exercised all the time.
“If she was waiting for the bus, she would be pacing in circles trying to get all her steps in,” remembers mom. “It was scary to see our child as sick as she was.”
Looking back, the patient remembers a pivotal moment when things really started to change.
“I went to a birthday party and we had cake. I went home and felt so gross. I decided from then on, I would start changing,” she said.
When she was 13, about a year after that birthday party, the patient’s family brought her for an assessment at MCH.
She was admitted to the inpatient eating disorders program that same day, which is the typical patient journey for those deemed to be too medically unstable to return home. She stayed for almost four weeks.
The diagnosis deeply impacted the entire family.
“I think it was quite rough for them. My siblings didn’t really understand what was going on. My mom ended up sleeping on a chair with me for the first couple of nights,” the patient says. “The nurses gave our family a book explaining what was going on so that was helpful.”
That was in June 2019. Over the next couple of years, she would continue to have follow-up visits with a social worker, a dietitian and her doctor.
“You are separate from your eating disorder.”
Inpatient program at MCH
Staff in the program gave her clear messages and strategies to manage her mental and physical health.
“And so the message of hope is that it’s possible to get yourself back,” says the patient. “You are separate from your eating disorder.”
She also remembers how kind the staff were.
“Whenever my parents weren’t there, they would come keep me company. I still remember some of the conversations we had and I use them for motivation to stay recovered even today,” she says. “Whenever I needed something, they were always there to get it. One of them painted my nails and another braided my hair. They were amazing.”
Meals were a stressful time, says her mom, but she learned to imitate some of the strategies she learned from staff in the program at home, such as distraction or giving her daughter a sensory fidget toy like putty to play with in her hands.
“They gave me a lot of support with meal times,” remembers the patient. “They had to sit in but they always knew what to do. Sometimes they would put on a show with me, other times they would talk with me through it.”
“I did not want to start the program at all,” she says. “But now, I’m very happy I went because I don’t know how things would be today. I feel like that was ultimately what initiated the change.”
“A very important step”
The patient had her last doctor’s check-up in November 2021 to complete the program. She is doing very well, and will continue to see a counsellor outside of the MCH eating disorders program.
Her family is very proud.
“It was really nice to focus on my daughter and not have to fight for her care. The program was ultimately a very important step in her pathway to healing,” says her mom. “Thanks to the great care we received at MCH, eating disorders are now part of our history and not our everyday life. And that’s something to celebrate.”