Introducing…lactation consultants
One of the most important skills a new parent must learn is how to feed their baby. Our lactation consultants are there to do just that – they help families feed their newborn by breast/chestfeeding or other appropriate methods when needed.
Early intervention with lactation consultants can greatly improve breast/chestfeeding success and help parents understand normal infant feeding cues.
Lactation consultant Camilla Aviss shares why having this role available after birth is so crucial to supporting new parents.
What is a lactation consultant?
Here at Hamilton Health Sciences’ (HHS) McMaster University Medical Centre (MUMC), International Board Certified Lactation Consultants (IBCLC) are all registered nurses (RNs) who have a background in maternal-child health with additional education and training over several years in complex breast/chestfeeding management. IBCLCs must pass an intensive international board exam and re-certify every five years with continuing education in order to maintain competency in breast/chest-feeding management skills.
IBCLCs support all infant feeding needs, not just breast/chestfeeding. These include feeding human milk using assistive devices like tubes, cups, spoons and bottles when necessary, how to use a breast pump, and how to use human milk substitutes such as formula when required. IBCLCs also work in a variety of other areas, such as public health, private practice and community clinics.
Approximately 3,000 babies are born at HHS sites each year. We are happy to support parents reach their feeding goals. Getting support early on can help ensure parents meet their goals and know where they can go for continued support in the community
What does your role entail?
Our role in the hospital is supporting new parents in establishing breast/chestfeeding after delivery and up to and including the first week of life. IBCLCs also share their knowledge with other members of the healthcare team and are involved in creating policy that supports breast/chestfeeding as the biological norm.
Currently MUMC has IBCLCs who support the women and newborn program (including the postpartum unit and intensive care unit), as well as pediatric units and the emergency department at McMaster Children’s Hospital, which is part of the same building.
Some of the more common reasons an IBCLC may be included in a care team to support feeding are painful feeds (breast/chestfeeding should not be painful), infant weight gain concerns, tethered oral tissues (commonly known as tongue ties), a parent with previous breast/chest surgery, endocrine disorders, or milk supply concerns.
How is feeding approached at MUMC?
Our approach is family-centred care. This means that you, your baby and your family are the focus of our care. We care for you together, so that you and your family can form a strong bond with your baby.
We support the World Health Organization’s recommendation of exclusive breast/chestfeeding for the first six months of life with continued breast/chestfeeding up to age two and beyond as mutually wanted by parent and baby.
What are some challenges when it comes to breast/chestfeeding?
One of the biggest challenges for parents is obtaining correct evidence-based information on infant feeding and having a supportive circle of care once home to help them meet their feeding goals. Community feeding supports such as Hamilton Public Health, private practice IBCLCs and community breast/chestfeeding clinics are key to this.
Many breast/chestfeeding parents benefit from joining peer support groups such as La Leche League Canada to connect with other parents and talk about breast/chestfeeding and adjusting to life as a new parent.
It is everyone’s responsibility to help support a parent’s feeding goals, starting before birth with breast/chestfeeding education and continuing after birth. Patients are referred to IBCLCs by the nursing and medical staff when complex feeding issues arise.
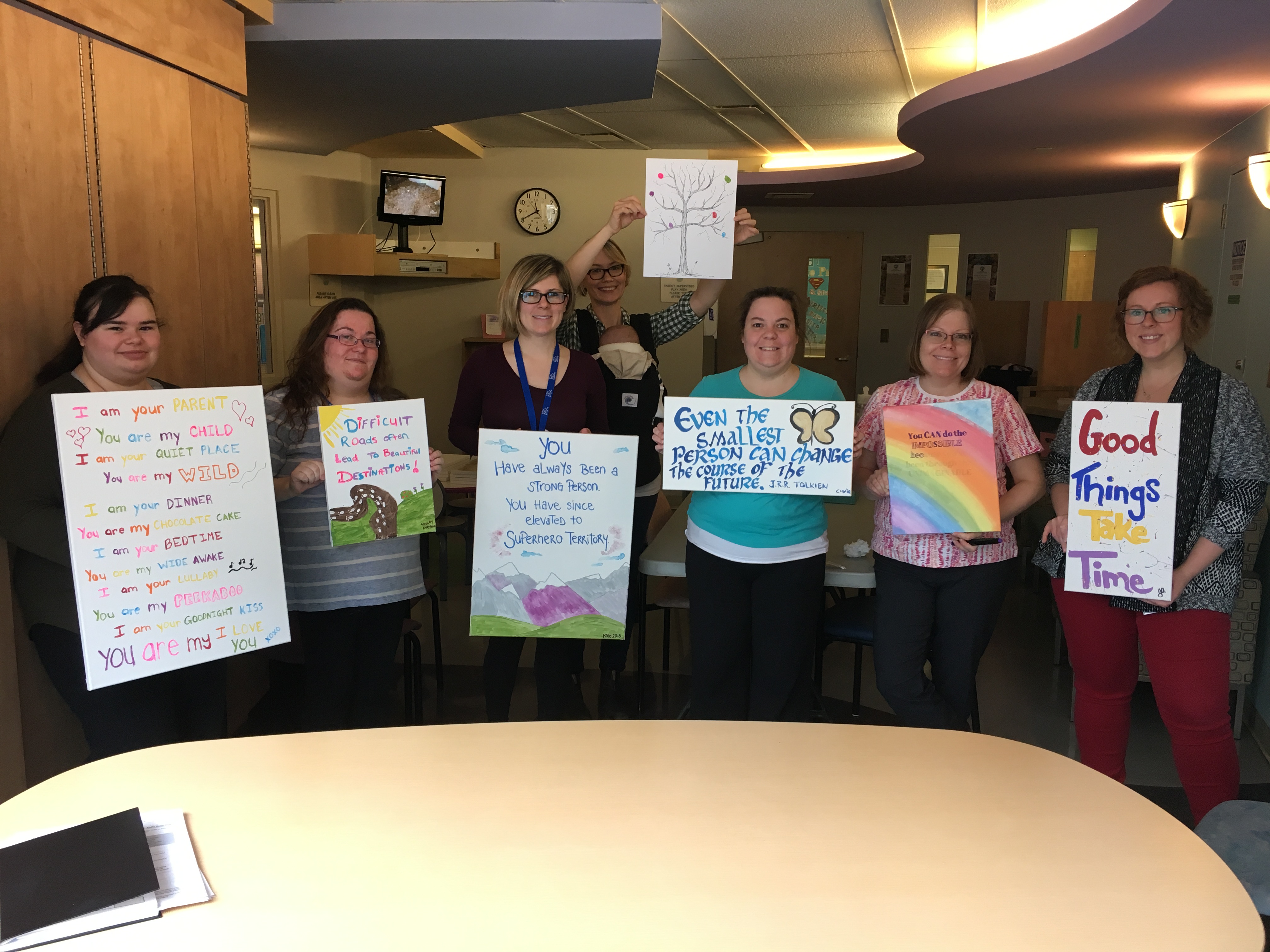
Meet some of the IBCLCs

Camilla Aviss
Camilla Aviss
26 years as RN, 12 years as IBCLC
“I became an IBCLC after having a high-risk pregnancy with my own twins who I delivered at 33 weeks. I consulted several IBCLCs for support and found it really difficult to reach my feeding goals. I decided then that I wanted to support other parents during this critical time in a family’s life. I then started my four year journey of taking the required lactation education courses, and completing my internship, over 3000 hours at that time!
I have always enjoyed the preventative aspect of nursing care and health teaching in various other nursing specialties I have practiced in. Breast/chestfeeding affects a child’s life long health trajectory as well as that of the nursing parent. Because of this, it’s very rewarding knowing I am impacting a child’s future health outcomes.”

Ruby Guevara
Ruby Guevara
11 years as RN, 3 years as IBCLC
“Originally, I had been working in a Toronto neonatal intensive care unit as bedside RN and I often worked closely with IBCLCs. With their guidance and mentorship, I was able to attain my clinical experience hours, education and pass my exam. Since then, I have transitioned to working in the maternal-child unit at MUMC as an IBCLC.
I’ve always had a passion for working with women, children and their families. A large part of the job is patient education but it’s also providing emotional support to families through their breast/chestfeeding journey. Celebrating the smallest of milestones with families feels amazing. Becoming an IBCLC felt like a natural fit.”

Renee Hildahl
Renee Hildahl
12 years as RN, 1.5 years as IBCLC
“I have always worked in maternal-child health and in my various nursing roles, quickly recognized the importance of breast/chestfeeding and consistent support for families to meet their feeding goals. I wanted to be equipped with the skill set and knowledge base for troubleshooting the many feeding related challenges that can occur families – becoming an IBCLC was the next right thing for me!
I was drawn to the role of lactation consultant as it encompasses a beautiful combination of teaching, assessment, and therapeutic skills. I love empowering parents to meet their feeding goals, overcome feeding challenges, and fostering important attachment within families. As a lactation consultant, I am able to equip parents with important education and practical strategies to help overcome potential challenges and instill confidence within the vulnerable transition to parenthood or adding a new baby to the family.”
Resources
Ontario Breastfeeds website
Hamilton Public Health resources