HHS researcher leads uniquely Canadian blood cancer study
Hamilton Health Sciences (HHS) hematology oncologist Dr. Hira Mian believes Canada has the potential to become an international leader in research into the treatment of multiple myeloma, a rare blood cancer.
“This trial has the potential to change the standard-of-care treatment in older adults with multiple myeloma not only in Canada but around the world.” — Dr. Hira Mian.
A large national clinical trial backed by $4 million in funding, which Mian is leading as the national study chair, could be the first step towards making this vision a reality. The MY13 trial is looking at whether monthly treatments of the medication daratumumab can be cut from five years (60 treatments) to 18 months (18 treatments) with the same medical benefits but improved quality of life and fewer side effects for older patients.
Study’s benefits
Mian’s study has the potential to both improve patients’ quality of life and save the Canadian health-care system millions of dollars since daratumumab is a costly, publicly-funded drug.
Launched this year, the study is taking place at 30 sites across Canada, with 559 patients over the age of 70 taking part over the next four years. This will include 80 patients from HHS Juravinski Hospital and Cancer Centre (JHCC). Recruitment at JHCC started in February.

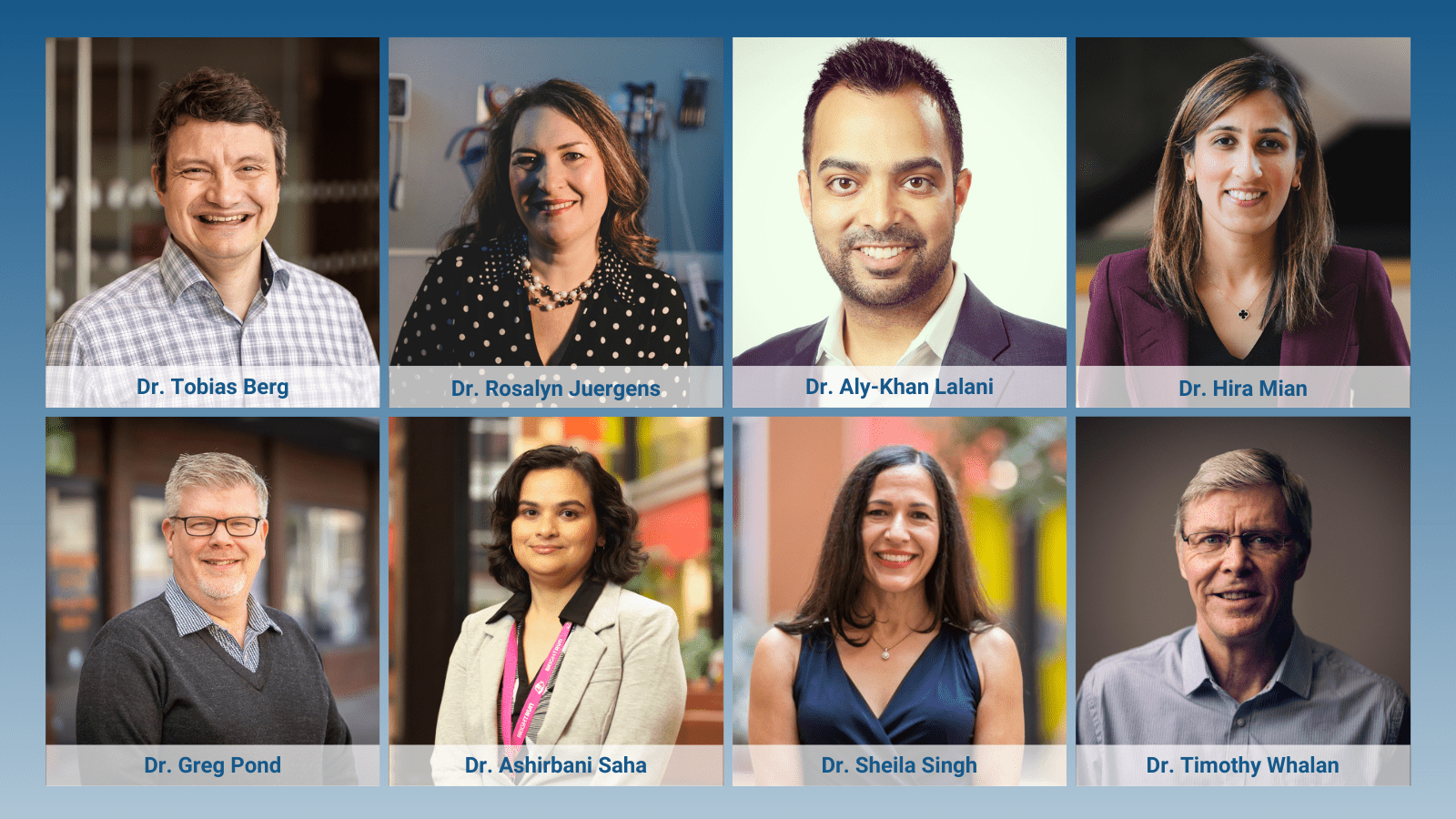
Dr. Hira Mian, national study chair
“This trial has the potential to change the standard-of-care treatment in older adults with multiple myeloma not only in Canada but around the world,” says Mian, who received funding from the Canadian Institutes of Health Research (CIHR) grant competition and Myeloma Canada, a non-profit organization for people living with multiple myeloma.
This trial will be conducted by the national Canadian Cancer Trials Group (CCTG) based in Kingston. The CCTG designs and conducts clinical trials that test cancer therapy, supportive care and prevention interventions across Canada.
“Multiple myeloma is a rare cancer, so it’s wonderful to get this level of funding,” says Mian, who is also a scientist with the Escarpment Cancer Research Institute (ECRI), a joint institute of HHS and McMaster University.
Mian divides her time between researching multiple myeloma and caring for patients at JHCC.
A rare cancer
About 4,000 people are diagnosed with multiple myeloma in Canada each year and they continuously receive treatment while in remission, which can last for years. During the first five years, the recommended, approved treatment is a combination of daratumumab — which is administered monthly at the hospital by IV or by injection – and two pill-form drugs that can be taken at home. The oral drugs are lenalidomide and dexamethasone. All three medications are publicly funded.
For the current standard of care, patients maintain this three-drug regimen for five years, as long as they don’t experience unacceptable side effects or a return of their cancer. It means that for five years, they’re travelling to a hospital every month for a treatment by IV or injection.
“This study is an excellent example of the leading-edge work being done by HHS researchers early in their careers, and it positions Canada to become a major force in multiple myeloma research.” — Dr. Marc Jeschke, HHS vice president of research and chief scientific officer.
“Five years is a long time to visit the hospital for monthly treatment, and daratumumab can also cause side effects including increased risk of infection,” says Mian. “It’s also a very expensive drug, costing the health-care system about $8,500 per patient, per month.”
Other studies indicate that patients don’t need continuous daratumumab for five years to receive the maximum benefit of this drug. Mian’s study further explores this, on a much larger scale, by cutting back daratumumab treatments to 18 months.
Recruiting patients
The trial divides patients into two groups. One group will receive the standard treatment of monthly IV or injection and two oral medications for five years. The other group will stop the IV or injection treatments after 18 months, with close monitoring, and continue with the oral medications.
The belief is that 18 months of daratumumab will be as effective as five years, and the overall goal is to have a safe and effective treatment available for older adults with newly-diagnosed multiple myeloma.
Why older patients?
Multiple myeloma patients receive constant treatment for the rest of their lives, and this can last for years. Five years of monthly IV treatments or injections especially impacts older patients, since it may mean spending the rest of their lives travelling to and from hospital every month.
“It’s a quality of life issue,” says Mian. “Throughout their whole disease course they’re constantly being treated with IV or injections in a hospital setting.”
For many patients, it means hours of travel time. In some remote northern communities, patients must be flown in monthly to the closest hospital offering this treatment.
While trials often involve a new drug, and new hope, this study cuts back on a drug that is proven to be effective in combination with the two oral medications. But Mian doesn’t expect this to hurt recruitment efforts.
“Patients have been eagerly waiting for this opportunity,” she says. “Going through IV or injections every month in hospital for five years really impacts quality of life. Instead, many patients welcome the opportunity to stop IV or injections after 18 months, knowing that preliminary data suggests they don’t need daratumumab for longer. They will also be carefully monitored.”
The study also gives older adults an opportunity to take part in research. “It’s a patient population that’s often excluded from trials for reasons including age or other existing health issues,” says Mian. “This trial lets them participate in research that has the potential to advance quality of life, especially for older patients like themselves.”
Growing an idea
Mian joined HHS as a hematology oncologist five years ago, after finishing her fellowship. She’s passionate about patient care, spending about 70 per cent of her work week providing direct care to patients. The other 30 per cent of her time is spent on research, which she finds hugely motivating because of the potential to improve patient care and outcomes for thousands of people nationally and globally.
The chance to lead a large national trial was an exciting opportunity, says Mian. “I really enjoy exploring new ideas and collaborating with researchers across the country.”
Five years ago, towards the end of her fellowship, Mian started to think about how the standard treatment of daratumumab with the two oral medications could be used more effectively, to improve quality of life, reduce side effects and bring significant cost savings to the health-care system.
As a new researcher, she considered leading a small study. But as the idea developed, it became clear that a large, national trial was needed to properly investigate this question.
“Dr. Mian is an exceptional oncologist and researcher,” says Dr. Marc Jeschke, vice president of research and chief scientific officer for HHS. “This study is an excellent example of the leading-edge work being done by HHS researchers early in their careers, and it positions Canada to become a major force in multiple myeloma research.”
Uniquely Canadian, eh?
Many other countries don’t publicly fund this drug combination, which puts Canada in a fairly unique position to run a large trial, adds Mian.
“We’re able to answer some of these bigger-picture research questions into multiple myeloma because of our health-care system and our population. The question posed in this study, about reducing daratumumab to 18 months, could likely only be answered in Canada.”
April is Cancer Awareness Month in Canada, a time to recognize our researchers, health care practitioners, volunteers, caregivers, policymakers, and community members who continue to innovate and advance cancer research and care across the country.
Cancer remains the leading cause of death in Canada. Today, there are 1.5 million Canadians living with and beyond cancer.