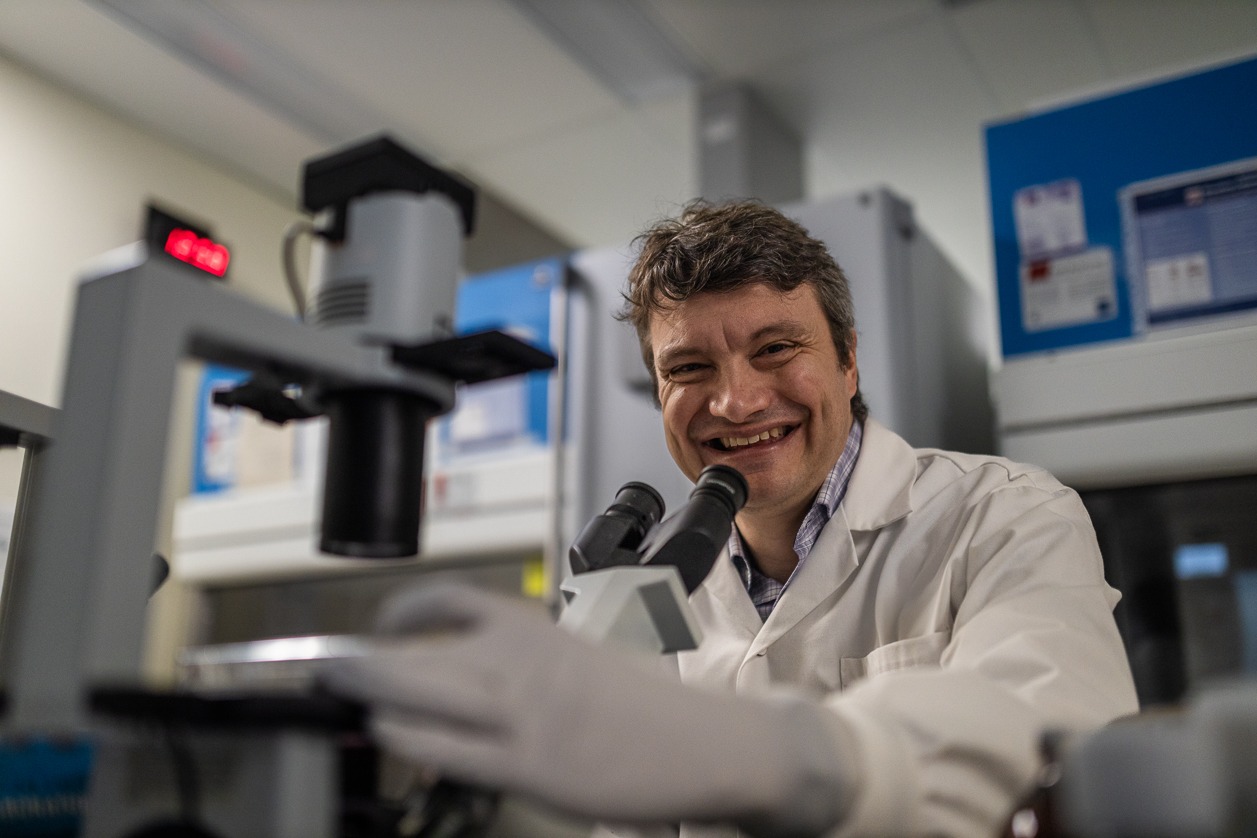
Studies improving care for prostate cancer patients, worldwide
Hamilton Health Sciences (HHS) researcher Dr. Gregory Pond is the lead statistician and co-investigator for two clinical trials that are transforming the way prostate cancer is managed, worldwide. Both multi-centre studies used magnetic resonance imaging (MRI) to improve the diagnosis and treatment for men going through a prostate cancer diagnosis.
MRI uses a powerful magnet and radiofrequency waves to make cross-sectional images that can show cancer missed by other tests. It can help identify the size and location of cancer and whether it has spread, and can help specialists plan treatments such as radiation therapy.
“This work is changing the diagnostic pathway, worldwide, for all men suspected of having prostate cancer.” — Dr. Gregory Pond.
The first study, called ASIST, ran from 2010 to 2015. It studied whether MRI found additional high-risk cancers when used in addition to the standard-of-care systematic biopsy, where 10 to 12 tissue samples are taken from random places in the prostate to check for cancer.
Due to the positive results observed in ASIST, a second study, called PRECISE, ran from 2015 to 2017. It studied whether MRI could determine if a biopsy was actually needed.
Improving how prostate cancer is diagnosed
One in eight men will be diagnosed with prostate cancer in their lifetime, making it the most common cancer to affect men in Canada, according to the Canadian Cancer Society.
Suspected cases of prostate cancer are typically identified through a prostate-specific antigen (PSA) blood test or rectal exam by a family doctor. In Canada and many parts of the world, a systematic biopsy — where 10 to 12 random tissue samples are taken using a needle and sent to a lab to testing and identification — is the standard of care for helping to diagnose prostate cancer.
Systematic biopsies are done using ultrasound to help guide where to take tissue samples from. Ultrasound uses sound waves to produce images, which can provide important information when diagnosing diseases like cancer.
“A biopsy is a very invasive procedure, and because these 10 to 12 samples are taken randomly, there’s still a risk of missing cancer,” says Pond, director of the Escarpment Cancer Research Institute (ECRI), a joint institute of HHS and McMaster University. Based at HHS Juravinski Hospital and Cancer Centre (JHCC), ECRI’s work focuses on research that has an impact on patient outcomes.
Biopsies can cause side effects including rectal bleeding, blood in the semen or urine, difficulty urinating, and infection including potentially-deadly sepsis in rare cases.
The ASIST and PRECISE studies are playing a major role in changing the pathway for these patients for the better, says Pond, who is also an associate director of the Ontario Clinical Oncology Group (OCOG) based at JHCC, which ran and sponsored both the ASIST and PRECISE trials.
““Dr. Pond’s outstanding work as lead statistician and co-investigator for these trials is improving patient care and transforming how prostate cancer is managed, globally.” — Dr. Marc Jeschke, vice president of research and chief scientific officer for HHS.
Running these trials required a large team at OCOG, says Pond, who is also a professor in the oncology department at McMaster and an Ontario Institute for Cancer Research (OICR) investigator. OICR is a cancer research and development institute dedicated to the prevention, early detection, diagnosis and treatment of cancer, with members across the province including in Hamilton.
Supporting academic research
Clinical trials are often funded by drug companies to test new medications. With no new drugs involved in the ASIST or PRECISE trials, there was no financial incentive for a drug company to get involved.
“That’s why these two studies really showcase the importance of having a group like OCOG to run trials,” says Pond. “These trials were completely academic, with the only incentive being to improve care for patients. In this case, there’s also a cost savings for government, but the ultimate goal was to help patients. These studies are excellent examples of why it’s so important to support academic research.”
ASIST-ing in finding the best pathway
ASIST was a randomized clinical trial involving 273 patients with prostate cancer. It aimed to determine whether using MRI in addition to a systematic biopsy guided by ultrasound could detect prostate cancer that was at risk of developing into aggressive disease at a different rate than when using ultrasound-guided biopsy process alone.
The study’s findings showed that MRI could potentially be used to help decide which patients would benefit from aggressive treatment versus which patients would be better suited for regular monitoring, since many prostate cancers aren’t aggressive.
PRECISE change for the better
PRECISE was a randomized clinical trial involving 453 men. It used MRI to determine that not all men suspected of having prostate cancer need to undergo a biopsy. In addition, using an MRI allowed for two to four tissue samples to be targeted, instead of 10 to 12 random tissue samples, meaning they were taken from areas that MRI identified as appearing cancerous. This targeted approach means that even in patients who do need a biopsy, it is less invasive, allowing for a faster recovery and fewer side effects.
As well as improving the ability to identify which men had high-risk disease, the study also helped lower-risk patients avoid radical treatment.
“This work is changing the diagnostic pathway, worldwide, for all men suspected of having prostate cancer,” says Pond.
Seventy-nine patients in this study, or 37 per cent, avoided a biopsy by first having MRI to check for signs of cancer and determine if a biopsy was needed.
“By providing MRI first, only those men who need a biopsy receive it,” says Pond. “It’s basically a win-win because we’re picking up the same amount of cancers as the systematic biopsy using ultrasound, but by doing the MRI first it’s safer, less invasive and more cost effective for the health-care system. Both studies have absolutely changed practice, and will continue to change practice worldwide.”
“These studies exemplify the cutting-edge research happening in Hamilton,” says Dr. Marc Jeschke, vice president of research and chief scientific officer for HHS. “Dr. Pond’s outstanding work as lead statistician and co-investigator for these trials is improving patient care and transforming how prostate cancer is managed, globally.
When the PRECISE study ended in 2019, researchers continued with a long-term evaluation, to see if over the following eight years there will be any change in the amount of cancer picked up. “After two years there was no change, but we’re continuing to monitor this over the long-term,” says Pond.
April is Cancer Awareness Month in Canada, a time to recognize our researchers, health care practitioners, volunteers, caregivers, policymakers, and community members who continue to innovate and advance cancer research and care across the country.
Cancer remains the leading cause of death in Canada. Today, there are 1.5 million Canadians living with and beyond cancer.